
Mostafa Elhennawy is pharmacy manager of the Seabird Island Pharmacy in Agassiz. Prior to this role, Elhennawy spent years working in remote northern BC communities such as Bella Bella, Terrace and Hazelton. Building a rapport with his clients remains his top priority: “There needs to be a relationship between pharmacist and patient. My patients need to trust me as a person before they can trust me as a pharmacist.”
Seabird Island Pharmacy in Agassiz is one of only a handful of retail pharmacies in BC located on and directly serving the community of a First Nations reserve. It was opened in March 2015 by Mohamed Hasanine and Tareq Youssef, who also own nearby Agassiz Remedy’s Rx.
Bordered by the Fraser River and surrounded by the scenic mountains of BC’s eastern Fraser Valley region, the Agassiz reserve is home to the Seabird Island Band, a thriving community hub with nearly 1,000 members and dozens of on-site services, including a daycare, K-12 community school, early childhood development programs, health and wellness programs, a dental clinic and medical clinic. Up until last year, however, those services did not include a pharmacy.
“We approached the band office to ask about a pharmacy because it was evident there was a need for this service on site,” says Mostafa Elhennawy, pharmacy manager of Seabird Island Pharmacy. “While downtown Agassiz is only an eight to 10-minute drive, it can be an hour-long walk for those without transportation. There was a real problem with medication adherence because it was so hard to provide this pharmacy service for patients if they didn’t have a reliable way to go into town.”
Elhennawy says the help and support of the Seabird Island Band was essential to establishing the pharmacy, in particular Chief Clement Seymour and Carolyne Neufeld, the director of health and social development.
Almost immediately, the pharmacy was bustling with patients, referred by the busy medical clinic located next door. While the compounding pharmacy offers a full range of clinical services, a large portion of time is dedicated to comprehensive, one-on-one medication reviews, in order to improve medication adherence, and therefore, health outcomes for patients.
“We found many people didn’t know exactly what medications they were taking and why,” says Elhennawy. He noticed patients would sometimes skip their medication for weeks at a time if away from home or unable to get to the nearest pharmacy for a refill. “When I came here, I started working one-to-one with the doctors and nurses to better serve our clients’ needs,” he says.
Within the year, medication adherence has jumped to more than 80 per cent, Elhennawy estimates. He says this is a direct result of the unique interdisciplinary health-care model being practiced in the Seabird Island community, which involves daily face-to-face interactions between doctors, nurses and pharmacy staff.
“This integrated health-care team is something I’ve never had before,” adds Dr. Marcella Beaulieu, a physician with the Seabird Island Health Centre.
Adherence – and continuity of care – is great with our pharmacist right here. To see our pharmacist and to work with the team directly is much more reliable for our patients’ needs.”
Dr. Beaulieu notes that to best serve the health needs of a primarily First Nations community, health-care practitioners need a widespread knowledge of the First Nations Health Benefits program (formerly Canada’s Non-Insured Health Benefits program or NIHB) to ensure medication coverage. Pharmacists also need in-depth knowledge on some of the most common health concerns affecting the community, such as diabetes. For the Seabird Island Health Centre, this includes operating a mobile diabetes team that pays regular home visits to patients, using state-of-the-art diabetes medicine and working closely with the pharmacy team on medication and overall health management.
“We’re working together to create an action plan for each patient to get the best results,” notes Elhennawy. “We’ve started to see a lot of real success stories in the last six months, especially from patients with diabetes. It takes time for people to build a rapport with you and try new things to see a difference in their health. It’s not just about taking pills, it’s about a lifestyle.”
For Elhennawy, who has spent years working in remote northern BC communities such as Bella Bella, Terrace and Hazelton before settling in the Fraser Valley at Seabird Island Pharmacy, building a rapport with his clients remains his top priority. “There needs to be a relationship between pharmacist and patient,” he says. “My patients need to trust me as a person before they can trust me as a pharmacist. And once you’re in, you’re in.”
One practical way he works on this service model is through continuous self-education on topics such as traditional indigenous medicine, which he notes is a vital part of providing well-rounded Aboriginal health care. He regularly reads up on the subject and personally partakes in traditional herbal therapies for common ailments such as headaches and stomach troubles to better understand this important facet of medicinal treatment when developing overall drug therapies for his pharmacy clients.
“I’m not here to change my patients’ mindset,” he notes. “I’m here to work with them.”
Understanding Aboriginal health care

Seabird Island Pharmacy in Agassiz is one of only a handful of retail pharmacies in BC located on and directly serving the community of a First Nations reserve. Bordered by the Fraser River and surrounded by the scenic mountains of BC’s eastern Fraser Valley region, the Agassiz reserve is home to the Seabird Island Band, a thriving community hub with nearly 1,000 members and dozens of on-site services.
Pharmacists Larry Leung and Jason Min followed an unorthodox career path after graduating from the UBC Faculty of Pharmaceutical Sciences in 2010 and 2008 respectively. With a keen interest in Aboriginal health care, Leung and Min were paired up for a Community Pharmacy Residency at UBC that took them to Bella Coola for a six-week practicum to help develop clinical pharmacy services for members of the Nuxalk Nation.
“It opened our eyes to all of the great work being done,” notes Leung. “But we also saw the potential to collaborate with local health-care workers and pharmacists to improve medication use in the community.”
Rather than take on traditional community pharmacy jobs, the pair decided to start their own consulting business, Clinicare Pharmacists, in 2011. The business specializes in improving medication management services, including in remote BC communities, by working in partnership with local pharmacy staff, medical professionals, Aboriginal elders and community members.
“Our goal was all about the optimization of the patient’s therapies,” says Leung, who along with Min has travelled to Bella Bella, Mount Currie and other communities over the past five years. “The work that was being done was not unique – it’s what a pharmacist does. But some of these communities just didn’t have that service.”
While each community had unique needs specific to its population and location, there was often a common theme – a lack of time and resources. Pharmacies could often be one or two hours away from a reserve community, or were understaffed.
While Leung and Min strived to work alongside communities to help develop pharmacy services, the duo quickly realized they had very little information and few tools available to offer the culturally safe care they hoped to provide. The pair felt there was a critical gap for pharmacy students looking to expand their knowledge and understanding of Aboriginal health care.
“Pharmacists may lack the understanding of Aboriginal culture and be unaware of the current and multi-generational issues that have contributed to health disparities that we see,” says Min. “In gaining cultural understanding, competence and humility, pharmacists can do their jobs more effectively.”
After approaching UBC, the pair introduced an elective course for third and fourth-year pharmacy students called Pharmaceutical Care in Aboriginal Health, which addresses topics such as terminology, the impact of colonialism and residential schools on Aboriginal health, truth and reconciliation, and pharmacy-specific topics related to diabetes, substance abuse and mental health. In addition, they worked with Aboriginal partners at UBC to ensure pharmacy students receive mandatory content on Aboriginal health starting in 2015.
Today, the pair work at the UBC Pharmacists Clinic to continue providing medication management services to First Nations communities throughout BC on a larger scale, as well as local patients on site at the Vancouver university.
“We took a step back to ask ourselves, ‘What is the goal of what we’re trying to achieve?’” says Leung. “There are more than 200 First Nations communities in BC alone and we only collaborate with a handful; we knew that we wanted to help build pharmacist capacity to better serve the needs of these communities.”
Improving health-care services for all patients
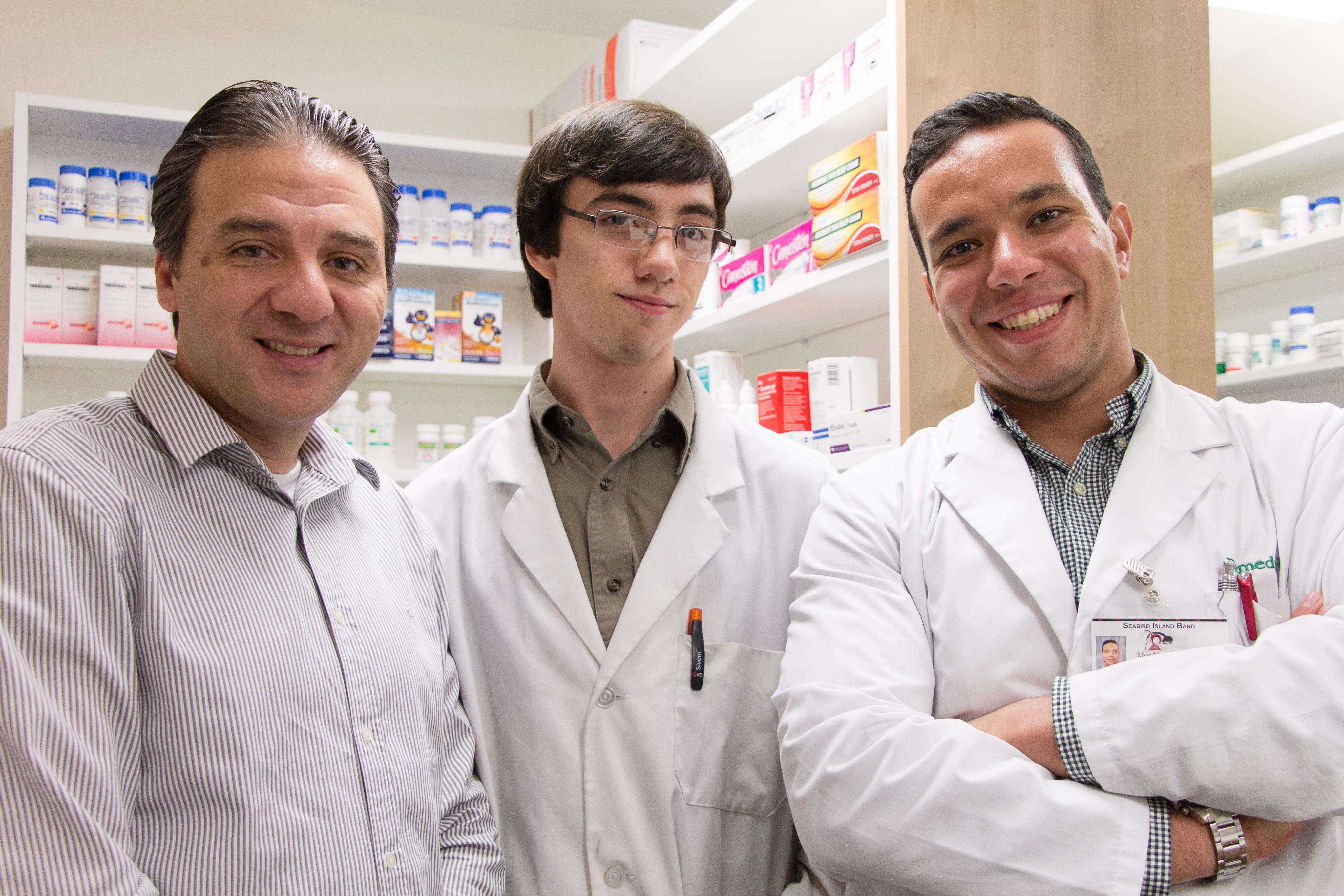
Tareq Youssef (left), co-owner of Seabird Island Pharmacy in Agassiz, with pharmacy assistant Ashton Penner (centre) and pharmacy manager Mostafa Elhennawy. Within a year of opening, Elhennawy estimates that medication adherence jumped to more than 80 per cent in the pharmacy. He says this is a direct result of the unique interdisciplinary health-care model being practiced in the Seabird Island community, which involves daily face-to-face interactions between doctors, nurses and pharmacy staff.

Despite health-care advancements across Canada, there is an overwhelming sentiment that remains strong among many health-care professionals – there is still much room for improvement when it comes to delivering pharmacy services to First Nations people.
A special session held August 20 in Vancouver on indigenous health, organized by the Indigenous Physicians Association of Canada, along with the Canadian Medical Association, the College of Family Physicians of Canada and the Royal College of Physicians and Surgeons of Canada, featured several recommendations from the Truth and Reconciliation Commission, including the need for specialized training on Aboriginal health issues as well as skills-based training in cultural understanding and humility.
“There is a definite power imbalance in the health-care system that needs to shift,” says Cindy Preston, senior pharmacy lead at the BC First Nations Health Authority (FNHA), the first province-wide health authority of its kind in Canada. “Even though there is good care going on, it can be better.”
Preston regularly travels to First Nations communities throughout BC to work with health-care teams to address and improve upon service delivery challenges, including pharmaceutical services.
She sees a huge opportunity for pharmacists to become leaders in the movement towards a health-care model that prioritizes cultural safety and humility for all patients. “Because we are a community-based entity, what an opportunity for the pharmacy profession to step up to start providing better care to all British Columbians.”
She cites the complexity of Canada’s colonial history, the multigenerational impact of residential schools on the health and wellness of Aboriginal people, and the deep-seated stereotypes that often plague the health-care system as barriers to providing culturally respectful health care.
“Developing cultural humility is the process of self-reflection to understand our personal and systemic biases as health-care providers,” says Preston. “Understanding that we as pharmacists don’t understand everything is a very key part to that.”
While there are no official certifications in Aboriginal health for pharmacists, all BC health-care providers are strongly encouraged by the FNHA to take the self-administered online San’yas Indigenous Cultural Safety Training developed by the Provincial Health Services Authority (PHSA) in 2010.
“Indigenous people are the fastest growing population in BC, yet experience the greatest inequities in health and access to care,” says Cheryl Ward, interim director of Indigenous Health and provincial lead of San'yas Indigenous Cultural Safety Training at the PHSA. “The training examines a range of complex issues and aims to increase knowledge, enhance self-awareness, and strengthen the skills of health professionals who work with indigenous people.”
To date, nearly 28,000 people in BC have completed the training, but only 158 pharmacists and pharmacy staff have opted in on the course.
“Pharmacy is a relationship-based practice,” says Preston. “The more that pharmacists can engage in cultural safety and humility, the more individuals will feel respected. That helps create a better health-care environment where all patients can feel safe and engage in those services more.”
To learn more about the PHSA San’yas Indigenous Cultural Safety Training course, visit sanyas.ca.
