Case: A young woman is prescribed metoclopramide for hyperemesis gravidarum. She is concerned about the boxed warning of tardive dyskinesia.
Pharmacists are often asked about the adverse effects of medications. Fear of side effects can be difficult for patients to understand leading to needless anxiety and even noncompliance. By knowing factors that cause the patient to worry excessively about side effects, pharmacists can help patients better weigh the risks against the benefits.
What is risk?
Risk is the combination of the side effect and its probability. Consider discussing: 1) The side effect 2) The probability of the side effect, 3) The potential benefit of the medication, and 4) Weighing the risk against the benefits.
What influences the perception of risk?
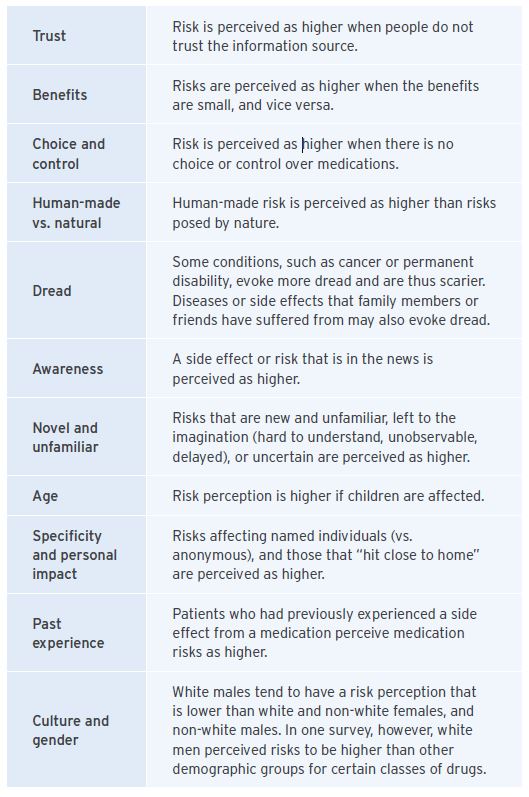
In addition to health literacy and numeracy, other factors can influence how patients perceive risks.
In our example, several of these factors are in play: there is heightened awareness (due to the boxed warning), unfamiliarity, and the effects may be delayed and potentially permanent. All this may be layered upon the heightened emotions of being pregnant.
Clear communication of risks!
The following tips can help pharmacists communicate information more clearly and help patients better understand their benefits and risks.
- Use plain language. Describing complex conditions can be a challenge, but there are a number of online resources that can help (e.g. MedlinePlus, WebMD).
- Sometimes the data is poor and our knowledge is limited. Maintain trust and acknowledge any uncertainty.
- Use numbers rather than phrases like “very rare”, “uncommon”. The following are regulatory definitions: very rare means <1 in 10,000 (including isolated case reports); rare means <1 in 1,000 but >1 in 10,000; uncommon (infrequent) means >1 in 1,000 but <1 in 100; common (frequent) means >1 in 100 but <1 in 10; very common: >1 in 10.
- Use frequency (e.g. two in a thousand) rather than percentages (0.2%).
- Keep denominators constant when making comparisons (e.g. the occurrence of tardive dyskinesia has been reported to range from 1 in 35000 prescriptions to 1 in 5000, but convert that to 3 per 100000 to 20 per 100000 prescriptions).
- Use absolute risks rather than relative risks. A 50% increase in the incidence of a side effect seems large, but the actual increase may be from two in a thousand to three in a thousand.
- Present the incremental risk (compared to baseline or placebo). Even pharmacists sometimes provide rates without the accompanying baseline rate, leading to inaccurate perceptions.
- Consider using graphs and pictographs to aid comprehension. There are free online programs that generate pictographs such as Cates plots (www.nntonline.net) and icon arrays (www.iconarray.com).
- Provide both positive and negative frames, e.g., “three in a hundred patients will develop a rash, while ninety-seven in a hundred will not.”
- Don’t forget to discuss benefits. Remember that patients perceive risks to be lower when the benefits are higher. The order in which information is presented can affect perceptions — if risks are discussed last, patients may focus on the risks.
- Individualize risk information when possible, considering the patient’s age, sex, health status, etc.
- Clarify the time interval over which a risk occurs or accumulates, e.g. the risk of tardive dyskinesia increases with therapy longer than 12 weeks.
As always, discuss monitoring, and be accessible when your patients have further questions or concerns!
References: Available on request.
