Local research aims to identify and reduce barriers faced by community pharmacists when providing care to patients recently discharged from hospital
By Shaylee Peterson, BSc(Pharm), ACPR, PharmD
It is well established that medication errors and adverse events occur frequently in patients recently discharged from hospital. Community pharmacists are often the first health- care professional hospitalized patients interact with after discharge, and are the first line of defense against medication-related problems. Unfortunately, there is limited information sharing between hospital and primary care providers, particularly community pharmacists, because of lack of integration with surrounding hospitals5,6. Community pharmacists have identified this as a barrier to them providing optimal patient care6-10. Internationally there has been discussion surrounding adding additional information to prescriptions15. For example, medical bodies in the UK, in particular, have made recommendations to include clinical indications on prescriptions16.
In B.C., discharge summaries from a hospitalization are typically sent to a patient’s primary care provider. B.C. also has eHealth Viewer (also known as CareConnect), which is an electronic health record that provides authorized caregivers the ability to view integrated clinical information from a variety of sources. Various clinical information is accessible on this record, including laboratory results, medical imaging and hospital reports depending on the health authority. Unfortunately, most community pharmacists in B.C. do not currently have access to this service.
We undertook a research study to determine the current barriers faced by community pharmacists in our community, as well as to determine their preferences for information provision at the time of patient discharge from hospital9. With the help of the BC Pharmacy Association, who was instrumental in helping us recruit participants, we conducted one-on-one interviews and a focus group with 12 community pharmacists in Kamloops.

Shaylee Peterson was part of a team who undertook a research study to determine the current barriers faced by community pharmacists in our community, and to determine their preferences for information provision at the time of patient discharge from hospital.
We found that the main barriers faced by participants caring for patients recently discharged from hospital included a lack of communication, incomplete prescriptions and limited clinical information. In addition to legal prescription requirements, three information items were identified as the most valuable to community pharmacists at the time of hospital discharge. These included laboratory values, hospital contact information and annotation of medication changes. The most frequently mentioned laboratory values that would be useful to community pharmacists were creatinine clearance and electrolytes. Annotation of medication changes refers to documenting that an intentional change was made to a previously prescribed medication, such as a medication discontinuation or dose change. We were surprised to find that one of the most commonly requested pieces of information was simply contact information for a care provider at the hospital, so a pharmacist could reach someone when needed for clarification. Participants felt that receipt of this additional information would improve their ability to provide timely and high- quality pharmaceutical care.
While several participants did mention the utility of documented medication indications or a medical problem list, we were surprised that this was not one of the most frequently preferred information items. Based on previously published literature, we had hypothesized this would be one of the most commonly requested pieces of information. Participants were also asked if they were concerned about any negative consequences associated with access to additional information, but most participants did not identify any concerns. Full results of the study can be viewed in the Canadian Pharmacists Journal.9
Now that we have completed our study and identified key information items desired by community pharmacists to help them improve the care they can provide, the more difficult question arises: how can we make changes to our current system to implement these results?
On a broader level, one obvious solution would be to improve access that community pharmacists have to clinical information. Authorizing community pharmacists to view resources such as eHealth Viewer would allow them to access desired information like recent blood work and discharge summaries when they felt it was necessary to care for their patients. Alberta currently has a similar electronic health record, Netcare, that community pharmacists have access to.
Providing similar access to B.C. pharmacists would be one possible solution. However, this would likely be challenging to implement, as it would require cooperation across several bodies and protocols in place to ensure security of patient information. Another action that could be undertaken by health authorities would be to update and implement novel discharge prescription templates to encourage inclusion of the identified information items. Typically, prescriptions are generated electronically from a patient’s in-patient medication administration record. This may allow for embedding of information such as serum creatinine for certain medications or prompts to include contact information or annotation of medication changes.
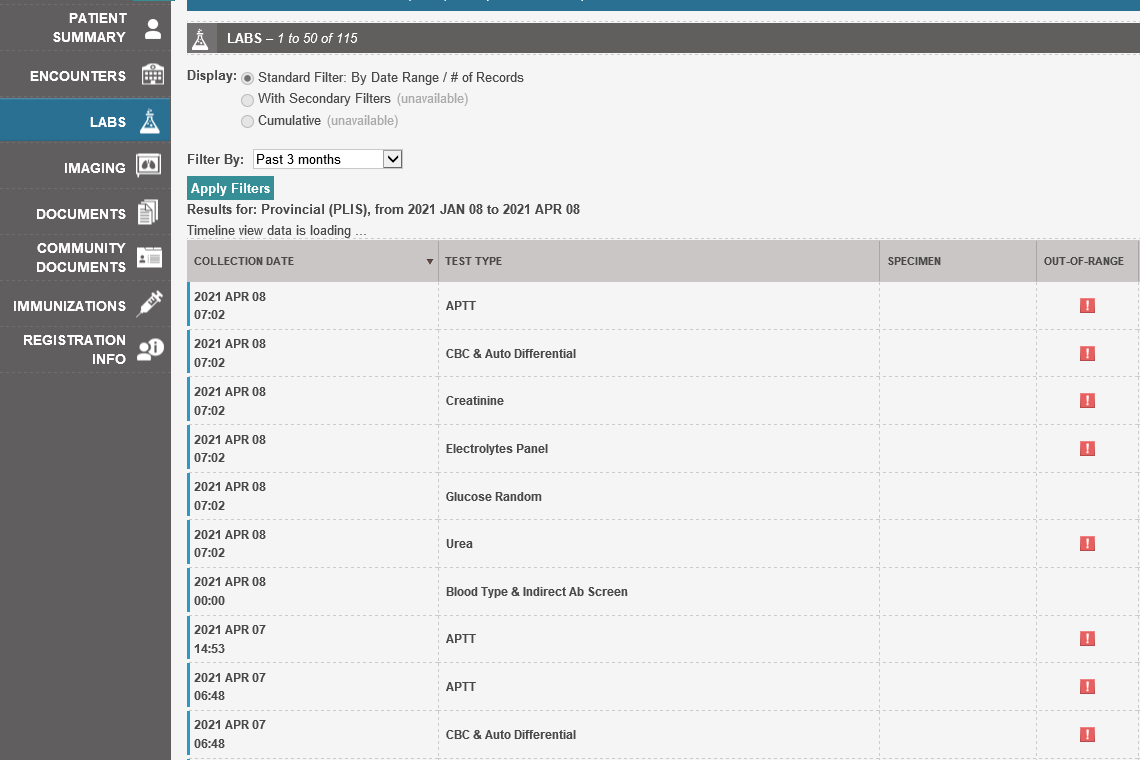
An example screenshot of CareConnect, an electronic health record system used in British Columbia that provides integrated clinical information.
Locally, in Interior Health and Kamloops, we will be taking various steps to translate the research findings into practice. We have a unique opportunity at Royal Inland Hospital (RIH) in Kamloops to make improvements via the ACE (advancing care electronically) initiative. With the ACE initiative, our currently paper-based hospital will be the first in Interior Health to switch to electronic documentation. We have been working with quality leaders to improve medication reconciliation with the new technology, and to ensure electronically- generated discharge prescriptions will meet the needs of community pharmacists.
Another unique form of documentation that may bridge the gap for community pharmacists has been developed and will be trialed with the ACE implementation at RIH; a pharmacists’ discharge summary. This discharge summary can be completed by a clinical pharmacist in the hospital and becomes a permanent part of the electronic health record that can be accessed on future admissions and can be copied to primary care providers and community pharmacies along with the discharge prescription. The template for this pharmacist discharge summary includes a list of medications continued, discontinued and adjusted along with the indication for the medication and rationale for the change. The template will also include any adherence issues identified and describe any suggested follow up or monitoring. Finally, it will include contact information for the clinical pharmacist. When completed, this summary would likely provide most of the information desired by community pharmacists.
However, we do not expect that this discharge summary will resolve all challenges community pharmacists face. Only patients with a clinical pharmacist involved in their care would receive one of the summaries, and in the near future this will be limited to a single hospital before the ACE project expands. Multiple interventions and practice changes will likely be required to ensure community pharmacists have access to all necessary information.
In summary, recent research conducted in Kamloops suggests that community pharmacists face challenges in providing care to patients recently discharged from hospital9. In this study pharmacists identified that additional information such as laboratory values, annotation of medication changes and hospital contact information would help them provide pharmaceutical care. Locally, we hope to implement changes to address these research findings. Our plans include the use of technology to improve documentation available to community pharmacists. More broadly, initiatives such as allowing community pharmacists in B.C. to access existing electronic health records could reduce barriers community pharmacists face and allow them to provide timely and comprehensive pharmaceutical care.
References
1. Munday A, Kelly B, Forrester JW, Timoney A, McGovern E. Do general practitioners and community pharmacists want information on the reasons for drug therapy changes implemented by secondary care? Br J Gen Pract 1997;47(422):563-6.
2. Zeleznikar EA, Kroehl ME, Perica KM, Thompson AM, Trinkley KE. Integration of community pharmacists in transition of care (TOC) services: current trends and pharmacist perceptions. J Pharm Pract 2017;089719001773597.
3. Brühwiler LD, Hersberger KE, Lutters M. Hospital discharge: what are the problems, information needs and objectives of community pharmacists? A mixed method approach. Pharm Pract 2017;15(3):1046.
4. Kennelty KA, Chewning B, Wise M, Kind A, Roberts T, Kreling D. Barriers and facilitators of medication reconciliation processes for recently discharged patients from community pharmacists’ perspectives. Res Soc Admin Pharm 2015;11(4):517-30.
5. Lounsbery JL, Green CG, Bennett MS, Pedersen CA. Evaluation of pharmacists’ barriers to the implementation of medication therapy management services. J Am Pharm Assoc 2009;49(1):51-8.
6. Redmond P, Carroll H, Grimes T, et al. GPs’ and community pharmacists’ opinions on medication management at transitions of care in Ireland. Family Pract 2016;33(2):172-8.
7. Schiff GD, Seoane-Vazquez E, Wright A. Incorporating indications into medication ordering—time to enter the age of reason. N Engl J Med 2016;375(4):306-9.
8. General Medical Council. Good practice in prescribing and managing medicines and devices. Good medical practice. Available: https://www.gmc-uk.org/ethical-guidance/ethical-guidance-for-doctors/prescribing-
9. Hambrook M, Peterson S, Gorman S, Becotte G, Burrows A. Medication management surrounding transitions of care: A qualitative assessment of community pharmacists’ preferences (MEMO TOC). Can Pharm J (Ott) 2020;153:301-307.
