Lyme disease (LD) in North America is caused by the bacterium Borrelia burgdorferi (Bb). Bb is transmitted in BC by Ixodes pacificus and I. angustus, a blacklegged tick found in valley regions of Vancouver Island, the Lower Mainland, the Sunshine Coast and the Interior. The most common tick found on humans in BC (wood or dog tick) does not carry Bb. In the rest of Canada (east of the Rockies) Bb is transmitted by I. scapularis. Reports of LD in Canada quadrupled between 2009 and 2013, likely due to the spread of ticks in eastern Canada as a result of climate change. The risk of LD in BC is low. Tick infection rates in BC have remained stable and low (<1%) compared to >20% in the northeastern United States.
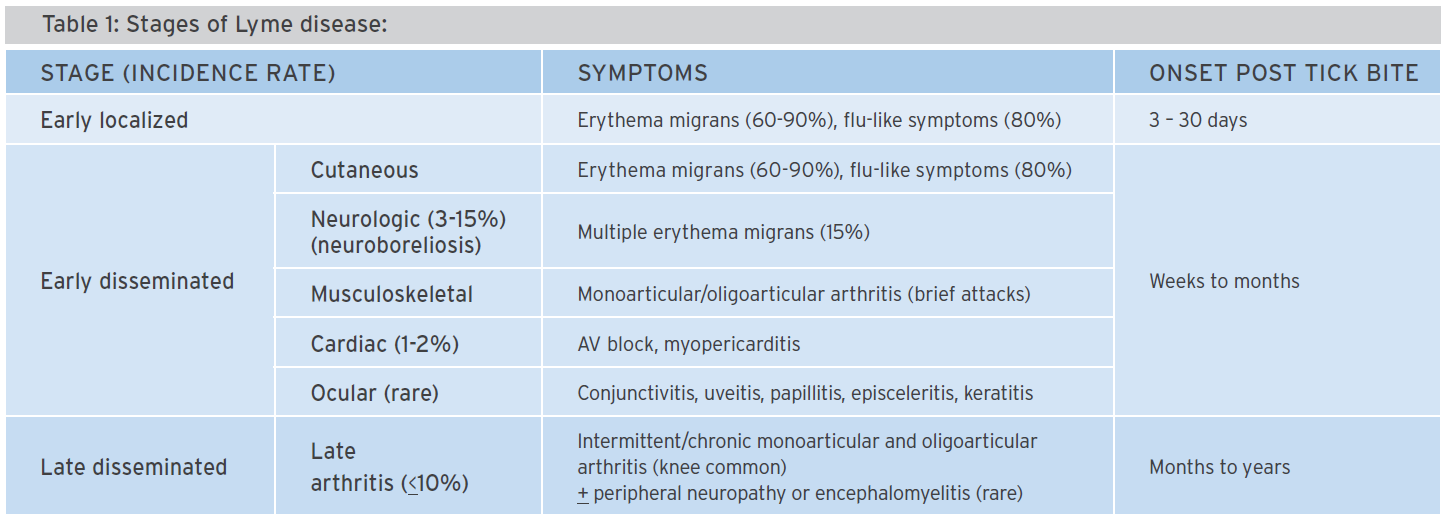
LD has three accepted clinical stages (Table 1). Early localized LD peaks in June to August and presents with an oval or round expanding rash (>5 cm) at the bite site, called erythema migrans (EM). EM is mostly homogenous; less than 10% have a bull’s-eye appearance. Differential diagnosis includes a bacterial infection at the bite site or a hypersensitivity reaction to tick saliva at the bite site usually within 48 hours, less than 5 cm in diameter and resolving within 48 hours.
Disseminated LD is diagnosed by antibody testing. It takes approximately two to four weeks for antibody testing to become positive and it may be influenced by prior antibiotic treatment. Antibodies remain high for many years so a positive test can indicate recent or remote infection.
Prophylaxis
Removing a tick within 36 hours of attachment (the time required for Bb to move from the blacklegged tick gut to it’s salivary glands) minimizes risk of LD. A single dose of doxycycline is 87% effective in preventing LD post-tick bite in areas of high tick Bb infection rates. Prophylaxis following tick bite in BC is not recommended due to low tick Bb infection rates (<1%).
Treatment
The Public Health Agency of Canada recommendations follow the Infectious Disease Society of America (IDSA) guidelines. The International Lyme and Associated Diseases Society (ILADS) recommend a longer course of antibiotics. Both recommend early treatment of acute localized LD because over 80% of patients treated for early LD have long-term complete resolution of symptoms. The IDSA recommends oral doxycycline, amoxicillin or cefuroxime axetil as first line and oral macrolides as second line treatment. Parenteral ceftriaxone, penicillin G or cefotaxime are recommended for meningitis, arthritis with neurologic symptoms or treatment-resistant arthritis. Length of treatment depends on LD stage (14-28 days). If antibody testing is indicated, patients should have samples drawn for testing prior to starting antibiotics.
Chronic Lyme disease
The existence of chronic LD remains controversial, but there is no compelling evidence that it is due to active or previous infection with Bb. Symptoms reported include fatigue, arthralgias, melalgias, paresthesias, insomnia and cognitive impairment. Post-treatment Lyme disease syndrome (PTLDS) is further differentiated from chronic LD where the former refers to symptoms that persist after antibiotic treatment for LD. The incidence of fatigue, cognitive impairment, insomnia, joint pain and numbness in chronic LD is increased in some studies, while others report no difference from controls. Four small and one moderate-sized randomized controlled trials reported little or no benefit of long-course antibiotics for fatigue, pain or neurocognitive function in PTLDS. The IDSA recommends symptomatic therapy (not antibiotics), whereas the ILADS recommends “considering” antibiotics with probiotics in patients with persistent symptoms of LD including using “higher doses, longer durations or combinations of first-line agents,” though this is based on expert opinion only. Some clinicians recommend adding metronidazole to the regimen to disrupt the ‘cystic form’ of Bb, despite no evidence of benefit or the existence of Bb cysts in humans.
Alternative treatments
There is no evidence for any of the following adjunctive therapies for LD: methyl B12 injections, Myers infusions (intravenous nutrient therapy), ribose powder, andrographis, eleuthero, glutathione, vitamin C, coenzyme Q10, alpha lipoic acid, vitamin B complex, vitamin B6, magnesium, omega-3, omega-6 and NT-factor.
Despite the controversy among various groups and guidelines, all emphasize careful differential diagnosis and evaluation for other causes. At the BC Women’s Hospital and Health Centre, a Complex Chronic Diseases Program has been set up to provide care for patients with chronic LD as well as other pain syndromes. Patients with symptoms compatible with chronic LD sometimes suffer for years, through countless clinical evaluations and tests without a proper diagnosis and effective treatment. It’s important that pharmacists understand the risks of contracting LD and the controversies concerning diagnosis, prophylaxis and treatment so that they can help patients navigate through the conflicting information.
References available on request at info@bcpharmacy.ca. Comments or DPIC article topic suggestions can be sent to info@dpic.ca.

