
Prefilled nasal spray can be used successfully by untrained individuals in high-stress situations and requires no preparation aside from opening the packaging.
Introduction
While the number of opioid fatalities continues to rise across Canada, the Canadian government is working in earnest to promote the use of lifesaving treatments by bystanders that can quickly counteract overdoses. Naloxone is an opioid receptor antagonist than can be delivered intravenously, intramuscularly or intranasally. Providing any form of this antidote to non-medical professionals has a great advantage because bystanders are typically the first people able to respond to opioid overdoses, potentially saving the lives of friends and family. However, considering that bystanders do not have several characteristics of trained first responders, such as health knowledge, emotional readiness and physical dexterity, designing devices that are easy for them to use presents unique challenges. These distinct needs must be taken into consideration.
The purpose of this article is to compare different methods of naloxone delivery and to provide evidence supporting Ontario’s decision in March 2018 to make NARCAN® nasal spray freely available to the public.1
Background
In Canada, the opioid epidemic began in the 1990s and continues to grow.2 The rise of opioid use in Canada reflects a change in prescribing habits after legal changes by Health Canada in 1996 that permitted more extensive use of opioids for pain management, with the thought that they were a low-risk, non-addictive, safe treatment for pain.2 In the mid-2000s, illicit drugs, including formulations using fentanyl, began appearing more frequently.2 These trends are associated with a rapid increase in death rates.2,3
There were approximately 3,000 opioid-related deaths in 2016, approximately 4,000 in 2017 and another 3,286 occurred between January and September 2018, 73 per cent of which involved fentanyl or fentanyl analogues.4 From 2010 to 2016, fentanyl deaths in six pan-Canadian provinces increased significantly and accounted for the majority of opioid-related deaths in British Columbia in 2016.5,6 British Columbia declared a state of emergency that year.2
Increase in synthetics shorten the therapeutic window for naloxone administration
Historically, opioid-overdose patients have tended to survive long enough for emergency medical services (EMS) to arrive. For example, results from a study published in 1996 conducted in the U.S. revealed that 84 per cent (609/726) of patients had a pulse when EMS arrived, and that 94 per cent (575/609) of those patients responded to naloxone.7 However, a study published in 2017 found that 90 per cent of fentanyl overdose victims did not have a pulse upon EMS arrival.8 An important difference is that an overdose with an opioid such as heroin typically occurs within 20-30 minutes of use,9 while fentanyl overdoses can occur within minutes or even seconds of use.8 Some estimates suggest that fentanyl and its derivatives are 50-100 times more potent than morphine, with one analogue, carfentanil, estimated to be 10,000 times more potent than morphine.10,11
Despite the difficulties associated with fentanyl, the national response-time goal in Canada for EMS to arrive remains eight minutes, 59 seconds for critical emergencies, but even this goal is only met 30 per cent of the time.12 In sum, the high potency and fast action of fentanyl in combination with the inadequate EMS response time signal a clear need for increasing the willingness and ability of bystanders to intervene and administer naloxone; however use of naloxone by bystanders is low.
Development of naloxone and historical use
Naloxone was developed in the early 1960s. In the early 1970s, it was being used to reverse the effects of anesthesia. By the mid-1980s, naloxone was used by medical emergency personnel in ambulances and hospitals as an antidote for reversing opioid/heroin overdose. Conversations regarding the use of naloxone by lay users began in the mid-to-late 1990s.13 In 2012, the BC Centre for Disease Control (BCCDC) began preparing for the BC Take Home Naloxone (THN) program.14 Around the same time, the United States Food and Drug Administration (FDA) held a workshop to examine the use of naloxone beyond clinical settings to reduce the number of deaths related to opioid overdose.15
The FDA hosted a public meeting in July of 2015 to discuss expanding both the accessibility and availability of naloxone.15 At this time, naloxone was only available as an injection (intravenous, intramuscular, or subcutaneous). As part of the expansion process, training on the proper use of naloxone was highlighted as a specific need.15 In the U.S., injectable formulations are often modified using nasal atomizers to allow off-label intranasal administration by Basic Life Support (BLS) EMS personnel as a non-invasive means to administer naloxone.16 The FDA approved NARCAN®, a nasal spray formulation of naloxone in November of 2015.17
Health Canada identified a need to increase access to alternative formulations of naloxone that are easier to administer.18 On July 6, 2016, the Minister of Health signed an interim order to allow NARCAN® prefilled nasal spray to be imported for one year while Health Canada completed an expedited review of the product to grant it normal approval on the Canadian market.19 Health Canada granted approval in June of 2017.20
Human factors
Before a device receives FDA approval, rigorous testing is required, including Human Factors Validation Testing, with the goal of ensuring “that the device user interface has been designed such that use errors that occur during use of the device that could cause harm or degrade medical treatment are either eliminated or reduced to the extent possible.”21 During testing, participants from a representative user population are provided devices to use in a real-world simulation. For example, usability testing with naloxone would include people who might witness an opioid overdose but have no medical training or background.22,23 The results must demonstrate that the device is safe to use and that it effectively delivers the medication as intended.
The combination of psychology, engineering and design is called Human Factors (HF) and is specifically related to the cognitive, physical, emotional, perceptual and behavioral aspects of a human. When designing a product, HF must be considered, especially in relation to what impacts the environmental situation has on the use of the device.24 User-centered design is closely associated with HF and focuses on the very specific type of person who will be using the product.25 Key considerations for bystanders who might observe an overdose and, ideally, deliver a dose of naloxone, include emotional distress and the likelihood that they also may be under the influence of a substance. The HF validation testing for the naloxone pre-filled nasal spray specifically evaluated the ability of individuals to use the product in this circumstance.
The results of the validation testing for FDA approvalshowed that 91 per cent (48/53) of participants were able to successfully administer a dose of the medication to a manikin simulation of an unconscious person.22 Of the five participants who were not successful, three of them appeared to have been confused by the manikin, however, they stated that they would be able to administer the drug successfully in the “real world.” Thus, the rate of successful administration was very high, even without training or instruction. Since an individual experiencing an overdose will likely die if untreated, any successful use of naloxone prefilled nasal spray means the possibility of a life saved. For both the FDA and Health Canada, the role of naloxone prefilled nasal spray in preventing death with little risk of harm was an important factor in their decision to approve it.
Participation of bystanders
Results from a survey of 100 opioid users regarding their experiences with overdose and naloxone use showed that while 68 per cent of participants had witnessed an overdose in the past, only 21 per cent saw a bystander administer naloxone. Although 65 per cent of participants accurately identified naloxone for opioid overdose reversal, only 33 per cent knew where to get the rescue kits.26 Additional research suggests that less than half of users reported having naloxone and, among those who had it, few had ever used it.27 These results highlight missed opportunities for bystanders to reverse an opioid overdose and begs the question, if users are aware of naloxone, and may even have it, why are they not using it?
Evidence indicates that a barrier to expanding access to the naloxone is the restriction of administration methods to injection-based administration.16 Research from McDonald, et al. validated this claim and showed that a layperson’s unfamiliarity with needle-based devices and fears of needle-stick-related injuries deters their use of needle-based devices such as injectable naloxone.28 Also, the World Health Organization (WHO) suggested that training for naloxone kits should not be mandatory, since a need for training may be a barrier to provision.29
Despite evidence showing that access to naloxone kits and bystander training reduces the number of opioid-related deaths,13,26 several barriers exist for proper administration, including complicated assembly. It follows that there is a need for a product that is easier to use and less intimidating. NARCAN® (naloxone prefilled nasal spray), which was approved by the FDA in 2015 and by Health Canada in 2016, may provide an alternative as it is needle free and can be used effectively without training, as discussed above.
Comparing intramuscular and intranasal options
In 2017, the Canadian Agency for Drugs and Technologies in Health (CADTH) conducted a review and found that the intramuscular (IM) and intranasal (IN) formulations of naloxone were both effective in reversing an opioid overdose.30 The review also cited the potential benefits of IN naloxone in reducing the risk of needle sticks in a potentially at-risk population for blood-borne diseases.30 The following summarizes the difference between IM and IN administration as well as the difference between two IN products—naloxone PFS with nasal-atomizer adapter kit and naloxone prefilled nasal spray.
Eggleston et al. compared the rate of successful administration of IM naloxone, multi-step atomized nasal naloxone and single-step naloxone prefilled nasal spray by community members in a simulated-use scenario.31 The authors found that, after completing a two-minute training video, community members were able to correctly administer the single-step naloxone nasal spray significantly more often than IM naloxone and significantly more rapidly than both the IM and multi-step atomized nasal naloxone products.31 Another recent study comparing multi-step atomized nasal naloxone and single-step naloxone prefilled nasal spray found that the success rate of administration of the single-step product was higher compared to the multi-step product.31
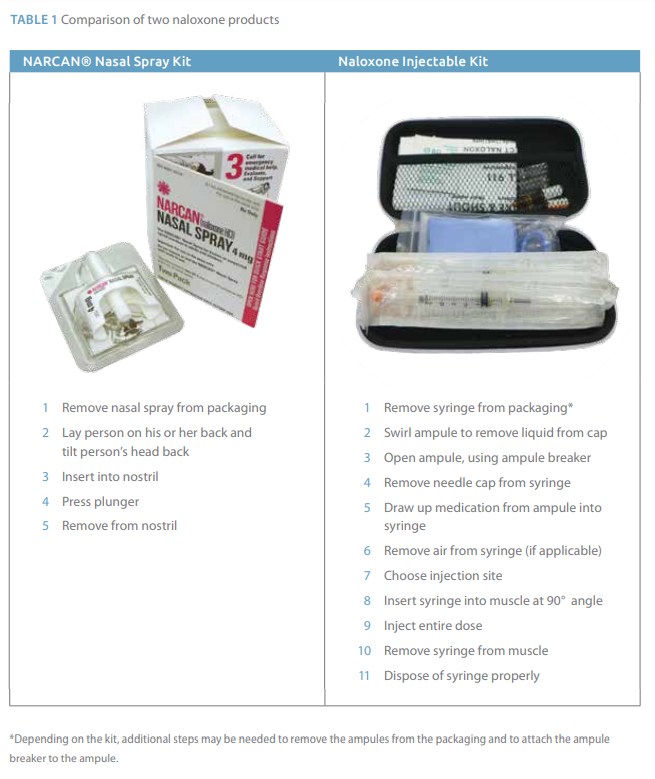
The key factor differentiating IM and single-step IN options is the number and difficulty of the tasks required to administer the respective products. Table 1 summarizes the steps required to use NARCAN® prefilled nasal spray and a naloxone injection kit. Because the prefilled nasal spray device requires fewer steps (half of those required for the PFS with nasal adapter), it is ideal for emergency situations, since each additional step takes time and leaves room for error. An in-depth task analysis of both options revealed that the simple design of the prefilled nasal spray is well suited to meet bystander needs.32
Discussion/Conclusion
As the use of synthetic opioids such as illicit fentanyl continues to rise, so do opioid-related deaths. Since overdose with fentanyl can occur within minutes, the window of time to react to an overdose has become very narrow and administration of naloxone by EMS alone is no longer sufficient. It is crucial that bystanders have an active role in naloxone administration, however they have unique needs. Prefilled nasal spray can be used successfully by untrained individuals in high-stress situations and requires no preparation aside from opening the packaging. It is dramatically more usable and has a more simple design compared to the naloxone injectable kit. Increased usability may result in a much better chance of successful reversal of an opioid overdose.
ABOUT THE AUTHORS Design Science is a human factors medical device consulting company with over 25 years of experience. The lead author, Mary Yovanoff, has an M.S. in Industrial Engineering with a focus in Human Factors from Penn State, a B.S. in Psychology and a B.S. in Mechanical Engineering. The authors have over 20 years of combined experience conducting studies in Human Factors.
ACKNOWLEDGMENTS The Authors would like to acknowledge Stephen B. Wilcox, Larry McGrath and David Grosse-Wentrup for their contributions to the article including minor edits, revisions and background research.
FINANCIAL ACKNOWLEDGEMENTS: Funding for this article was provided by Adapt Pharmaceuticals.
References
1. Fraser K. Spike in opioid deaths prompts Ontario government to offer free naloxone spray. 2018; https://www.cbc.ca/news/canada/windsor/ontario-opiod-death-spike-free-nalaxone-1.4567224. Accessed April 1, 2019.
2. Howlett K. Canada's opioid crisis. 2018; https://www.thecanadianencyclopedia.ca/en/article/canadas-opioid-crisis. Accessed April 1, 2019.
3. Canada SCoHotHoCo. Report and recommendations on the opioid crisis in Canada. 2016; http://publications.gc.ca/collections/collection_2016/parl/xc62-1/XC62-1-1-421-6-eng.pdf. Accessed April 1, 2019.
4. Special Advisory Committee on the Epidemic of Opioid Overdoses. National report: apparent opioid-related deaths in Canada (January 2016 to September 2018). 2019; https://infobase.phac-aspc.gc.ca/datalab/national-surveillance-opioid-mortality.html. Accessed May 9, 2019.
5. Canada H. Progress report on the joint statement of action to address the opioid crisis in Canada. 2017; http://www.ccsa.ca/Resource%20Library/CCSA-Addressing-Opioid-Crisis-in-Canada-Summary-Report-2017-en.pdf. Accessed April 1, 2019.
6. Fischer B, Vojtila L, Rehm J. The 'fentanyl epidemic' in Canada - some cautionary observations focusing on opioid-related mortality. Prev Med. 2018;107:109-113.
7. Sporer KA, Firestone J, Isaacs SM. Out-of-hospital treatment of opioid overdoses in an urban setting. Acad Emerg Med. 1996;3(7):660-667.
8. Somerville NJ, O'Donnell J, Gladden RM, et al. Characteristics of fentanyl overdose—Massachusetts, 2014-2016. Morbid Mortal Weekly Rep. 2017;66(14):382-386.
9. Fairbairn N, Coffin PO, Walley AY. Naloxone for heroin, prescription opioid, and illicitly made fentanyl overdoses: challenges and innovations responding to a dynamic epidemic. Int J Drug Policy. 2017;46:172-179.
10. O'Donnell JK, Halpin J, Mattson CL, Goldberger BA, Gladden RM. Deaths involving fentanyl, fentanyl analogs, and U-47700 - 10 states, July-December 2016. MMWR Morb Mortal Wkly Rep. 2017;66(43):1197-1202.
11. Morgan J, Jones AL. The role of naloxone in the opioid crisis. Toxicol Commun. 2018;2(1):15-18.
12. B. B, Ambulance Paramedics of BC. 2017; https://www.paramedicsin859.com/. Accessed April 1, 2018.
13. Rzasa Lynn R, Galinkin JL. Naloxone dosage for opioid reversal: current evidence and clinical implications. Therapeutic advances in drug safety. 2018;9(1):63-88.
14. British Columbia Centre for Dease Control. The history of community naloxone in British Columbia. 2017; https://towardtheheart.com/assets/uploads/15500816801BnKyWza9oKoKKxgoV1RTNg7smwaRoaHsTnNn27.pdf. Accessed April 1, 2019.
15. US Food and Drug Administration. Exploring naloxone uptake and use public meeting. 2015; https://www.fda.gov/downloads/Drugs/NewsEvents/UCM469456.pdf. Accessed November 19, 2018.
16. Wermeling DP. Review of naloxone safety for opioid overdose: practical considerations for new technology and expanded public access. Therapeutic advances in drug safety. 2015;6(1):20-31.
17. US Food and Drug Administration. FDA news release: FDA moves quickly to approve easy-to-use nasal spray to treat opioid overdose. 2015; http://wayback.archive-it.org/7993/20170111122937/http://www.fda.gov/NewsEvents/Newsroom/PressAnnouncements/ucm473505.htm. Accessed October, 2018.
18. Canada H. Frequently asked questions: access to naloxone in Canada (including NARCAN™ Nasal Spray). 2017; https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/announcements/narcan-nasal-spray-frequently-asked-questions.html. Accessed April 1, 2019.
19. Canada H. Interim order respecting naloxone hydrochloride nasal spray. 2016; https://www.canada.ca/en/health-canada/services/drugs-health-products/drug-products/announcements/interim-order-respecting-naloxone-hydrochloride-nasal-spray.html. Accessed April 1, 2019.
20. Canada H. Authorized Canadian naloxone nasal spray (NARCAN) coming to market [press release]. 2017; http://www.healthycanadians.gc.ca/recall-alert-rappel-avis/hc-sc/2017/63784a-eng.php. Accessed April 1, 2019.
21. US Food and Drug Administration. Applying human factors and usability engineering to medical devices: guidance for industry and Food and Drug Administration staff. 2016; https://www.fda.gov/downloads/MedicalDevices/DeviceRegulationandGuidance/GuidanceDocuments/UCM259760.pdf. Accessed November 19, 2018.
22. Krieter P, Chiang N, Gyaw S, et al. Pharmacokinetic properties and human use characteristics of an FDA-approved intranasal naloxone product for the treatment of opioid overdose. J Clin Pharmacol. 2016;56(10):1243-1253.
23. Tippey KG, McGrath LS, Yovanoff M, Sneeringer P. Moderating styles: understanding diverse techniques for investigating the root cause of use events. Proc Hum Fact Ergon Soc Annu Meet. 2018;62(1):605-609.
24. Schaeffer NE. The role of human factors in the design and development of an insulin pump. J Diabetes Sci Technol. 2012;6(2):260-264.
25. Wickens CD, Gordon SE, Liu Y. Design and evaluation methods. In: An Introduction To Human Factors Engineering. New York, NY: Longman; 2004:30-60.
26. Kirane H, Ketteringham M, Bereket S, et al. Awareness and attitudes toward intranasal naloxone rescue for opioid overdose prevention. J Subst Abuse Treat. 2016;69:44-49.
27. Heavey SC, Chang YP, Vest BM, Collins RL, Wieczorek W, Homish GG. 'I have it just in case' - naloxone access and changes in opioid use behaviours. Int J Drug Policy. 2018;51:27-35.
28. McDonald R, Campbell ND, Strang J. Twenty years of take-home naloxone for the prevention of overdose deaths from heroin and other opioids—conception and maturation. Drug Alcohol Depend. 2017;178:176-187.
29. World Health Organization. Community management of opioid overdose. Geneva, Switzerland: World Health Organization; 2014.
30. Peprah K, Frey N. Intranasal and intramuscular naloxone for opioid overdose in the pre-hospital setting : a review of comparative clinical and cost-effectiveness, and guidelines. 2017; https://www.cadth.ca/sites/default/files/pdf/htis/2017/RC0865%20Intranasal%20Naloxone%20Update%20Final.pdf. Accessed April 1, 2019.
31. Eggleston W, Podolak C, Sullivan RW, Pacelli L, Keenan M, Wojcik S. A randomized usability assessment of simulated naloxone administration by community members. Addiction. 2018;113(12):2300-2304.
32. Tippey KG, Yovanoff M, McGrath LS, Sneeringer P. Comparative human factors evaluation of two nasal naloxone administration devices: NARCAN® nasal spray and naloxone prefilled syringe with nasal atomizer. Pain and therapy. 2019.
