Sensor based technology in diabetes management
When pharmacists think about self-monitoring of glucose, there are generally three different types of technologies: the traditional capillary glucose monitoring method, interstitial fluid glucose sensors and interstitial glucose sensors equipped with transmitters.
Unlike traditional fingerstick glucose monitoring which measures capillary glucose, sensor based glucose monitoring measures interstitial fluid. This technology was first developed in the 1990s but has been evolving ever since and now multiple models permit patients to read blood glucose level continuously, allowing regular updates on blood glucose levels throughout the day, without drawing blood.
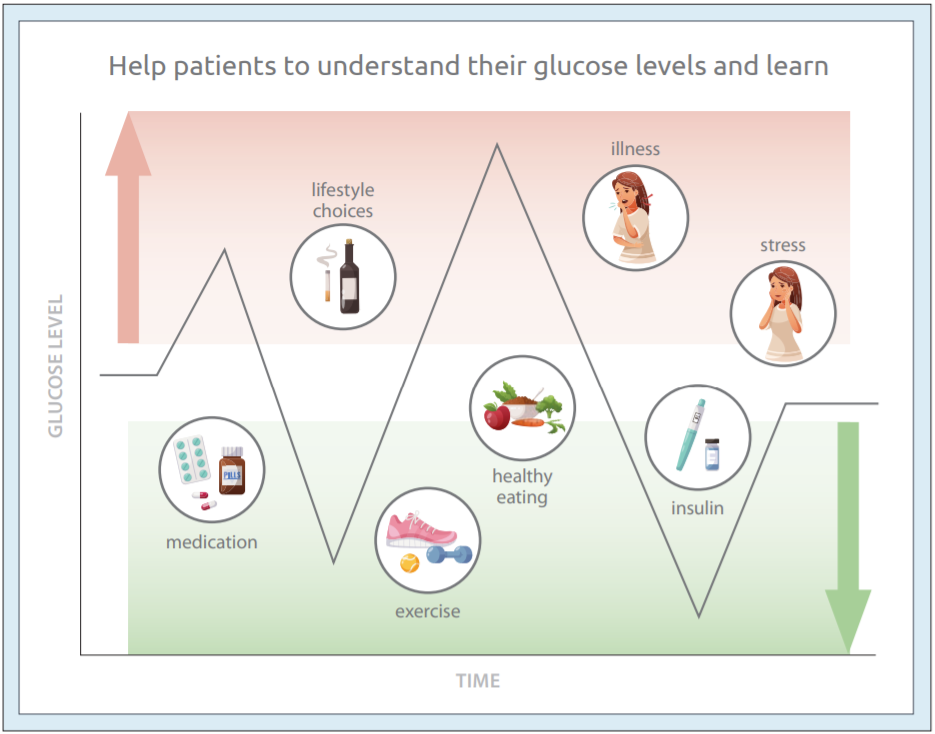
This enables patients and their pharmacists to gain a more wholesome view of their activities throughout the day and how their lifestyle choices, such as type of meals and level of physical activity, impact glucose levels.
For advertising inquiries, please contact angie.gaddy@bcpharmacy.ca
There are two types of interstitial fluid glucose sensors: real time continuous glucose monitoring (rtCGM), which proactively “pushes” the information to a reader, and flash glucose monitoring (FGM), also referred to as intermittently scanned continuous glucose monitoring (isCGM), where the data must be pulled from the sensor when a reading is needed.
rtCGMs can come as standalone devices or come integrated into an insulin pump with Bluetooth wireless connectivity, along with alarms that will trigger when glucose levels are too high or too low. Glucose levels are measured every minute and the glucose value is sent out – or “pushed” – every five minutes. The variable length of wear can be anywhere from five to 10 days and the data is stored in a cloud. Examples of this type of device include the DexCOM® G6 device and the Medtronic® Guardian Connect device.
Many pharmacists may already be familiar with the isCGM technology platform called FreeStyle Libre™ Flash Glucose Monitoring System. Unlike their real-time counterparts, which can communicate at a distance, isCGMs use near-field communication. That is, the reading device must be in close proximity to the sensor in order to obtain a reading. They provide 14 days of wear, no calibration is needed and readings are obtained by physically placing the reader close to the sensor or using a smartphone application to access the readings. Data is connected to the LibreView® cloud software where patients can access it. A recently approved version of isCGM now indicated for children four years of age and older, and is also equipped with high and low glucose alarms.
For pharmacists, it is recommended to set individualized target ranges in collaboration with the physician that are appropriate for the patient.
A completed line graph will appear on the reader screen for the patient using the device’s readings if the patient wears their continuous glucose monitor for at least eight hours. As the sensor measures glucose levels every minute, the patient is able to identify times during the day they are at target and also the impact of lifestyle choices such as diet and exercise.
Continuous glucose monitors are helpful in identifying a patient’s glucose level trend, and less effective at identifying whether a patient is hyperglycemic or hypoglycemic at a specific point in time. Continuous glucose monitors help the patient and their health-care provider do this by displaying “trend arrows” with their readings, providing five points of trend indication, based on the direction of the arrow:
![]() Directly up: an increase of blood glucose concentration of at least 1.5 mmol/L in the next 15 minutes if no action is taken.
Directly up: an increase of blood glucose concentration of at least 1.5 mmol/L in the next 15 minutes if no action is taken.
![]() Directly down: a fall of at least 1.5 mmol/L in the next 15 minutes if no action is taken.
Directly down: a fall of at least 1.5 mmol/L in the next 15 minutes if no action is taken.
 Diagonally up: a rise of between .9 and 1.5 mmol/L in the next 15 minutes if no action is taken.
Diagonally up: a rise of between .9 and 1.5 mmol/L in the next 15 minutes if no action is taken.
![]() Diagonally down: a fall of between .9 and 1.5 mmol/L in the next 15 minutes if no action is taken.
Diagonally down: a fall of between .9 and 1.5 mmol/L in the next 15 minutes if no action is taken.
![]() Horizontal facing: minimal change in glucose within the next 15 minutes.
Horizontal facing: minimal change in glucose within the next 15 minutes.
The patient will not only be equipped with their current glucose reading and the trend of where their glucose levels are headed in the next 15 minutes, but also how their glucose levels were affected by their choices over the past eight hours. The visual representation of glucose trends reinforces positive lifestyle choices and provides insights for when the patient is not in target range.
When a patient first begins using continuous glucose monitoring sensors, they should be reviewing their readings at least every eight hours. It is not recommended for patients who do not want to scan every eight hours.
Lastly, for patients, it may help to keep four things in mind when using glucose monitoring sensors:
- Scan frequently
- Learn from the trends
- Act and be proactive
- Do not react
Consider all these four different aspects to encourage the patient to learn from their results and be proactive in making changes to their lifestyle choices.
This article was written based on information from the BCPhA webinar “The Role of Technology in Diabetes Management” delivered by Pindy Janda, B.Sc Pharm, RPh on May 19, 2021.
As an accomplished clinical business development pharmacist with over 20 years of community pharmacy experience, Pindy has a proven track record in patient & pharmacist education, chronic disease management initiatives, pharmacy operations and business development. Pindy believes in empowering her fellow community pharmacists to maximize their expanded scope of practice resulting in improved patient outcomes for their patients and increased community pharmacy viability.
For advertising inquiries, please contact angie.gaddy@bcpharmacy.ca