
Community pharmacy prescription dispensing counts have reached more than 100 million for the first time in British Columbia, marking a significant milestone in the quantity of services delivered by the profession.
According to data provided by the B.C. Ministry of Health, community pharmacists dispensed 102.7 million prescriptions in the latest year, up nearly 45 per cent from 2015, when there were 70.8 million prescriptions dispensed. Even more notable, during that same period, B.C.’s population only increased 19.5 per cent, suggesting British Columbians’ need for pharmacy services is outpacing the population growth.
According to estimates from provincial statistics agency BC Stats, in 2024, B.C.’s population is estimated to have reached 5.7 million people, with a growing senior population of approximately one dependent senior, who often have more complex health needs, for every three people in the province’s workforce.
Pharmacists are busier than ever. In 2024, the average community pharmacist dispensed 24,000 prescriptions each, about 20 per cent higher when compared to 2015. In addition, the profession’s scope of practice has grown significantly in recent years, and the average pharmacist’s job has evolved far beyond dispensing medications.
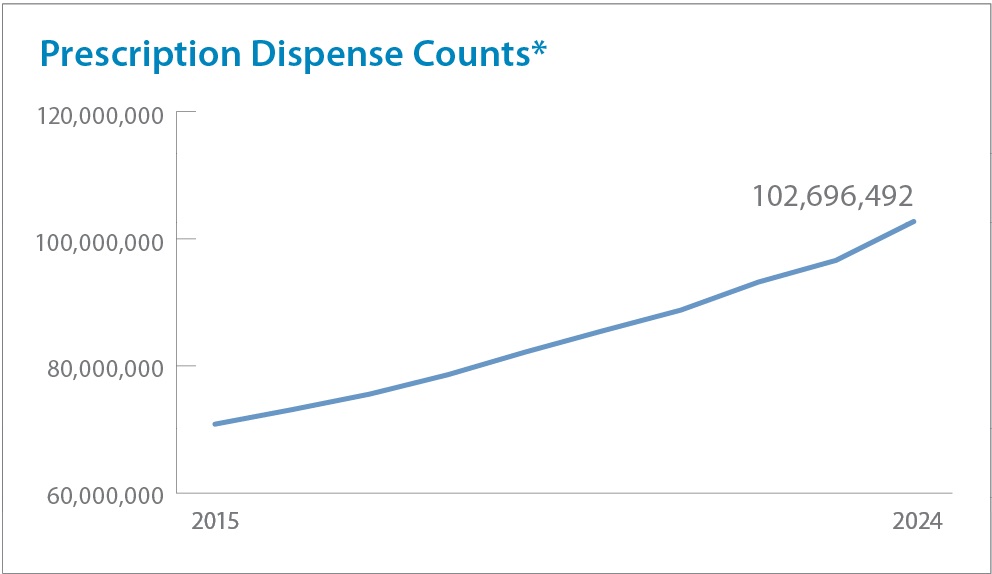
*Dispenses include drugs, medical devices and supplies dispensed primarily at community pharmacies.
The pharmacist’s role in administering vaccines and more
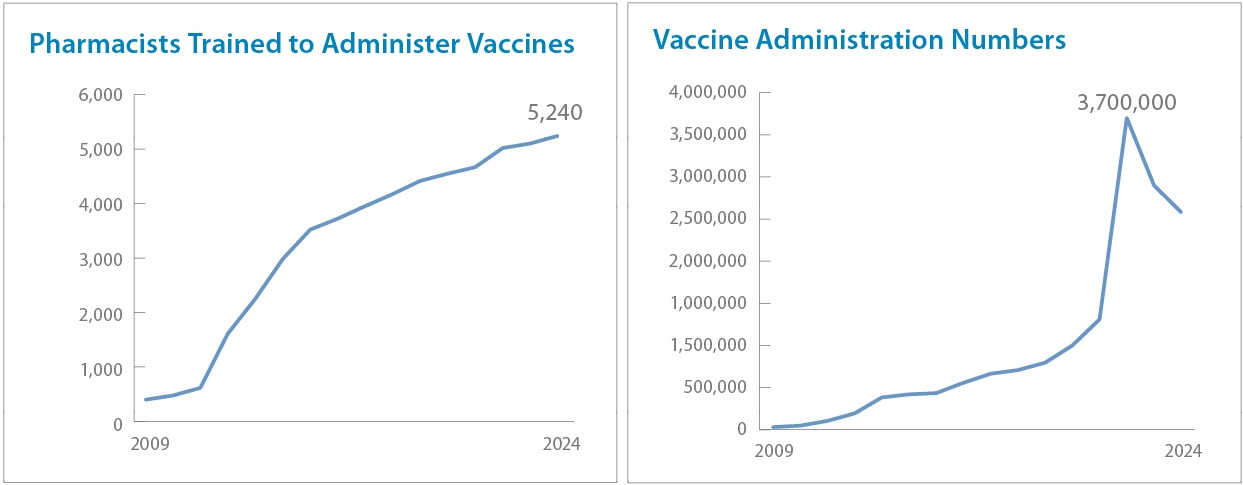
Since 2009, the British Columbian pharmacist’s scope of practice has been shifting towards increased clinical services that make health care more accessible while alleviating demands placed on other health sectors. In response to the H1N1 pandemic, pharmacists were authorized to administer vaccines, beginning with 31,000 influenza vaccines in 2009. All pharmacists in B.C. must complete an accredited training course approved by the College of Pharmacists of British Columbia, or have authorization from practicing in another province, before they can administer vaccines. In 2022, authorization was expanded to include injections for other medications, not just vaccines.
As acceptance of the new drug administration authority grew, the number of vaccines administered by pharmacists grew exponentially. As of 2024, more than 5,200 pharmacists and pharmacy students were certified to administer medications by injection or intranasally. In that same year, B.C.’s community pharmacists administered 1.25 million flu vaccines — a 40-fold increase from the initial year! And during the peak of the COVID-19 pandemic, community pharmacy administration of flu and COVID vaccines reached a staggering 3 million shots, with PharmaCare’s annual “Trends” report showing that funding for injection fees hit a high of $55 million in the 2022/23 fiscal year. This is a substantial amount, considering that same year, the total dispensing fees and long-term care service fees paid to pharmacies made up $289 million.
Ensuring patients have uninterrupted care using the most suited medication
2009, the same year that pharmacists were authorized to administer vaccines, also saw another substantial benefit to patients come into force — adaptations and renewals. This change gave pharmacists authorization to renew expired prescriptions for up to one year, saving patients trips to the doctor’s office, and enabled pharmacists to independently adapt medications by changing the dose, formulation or regimen, or making a therapeutic drug substitution within the same therapeutic class, to make sure that patients were receiving the most effective treatment.
With health-care resources stretched during the COVID-19 pandemic, in 2022, the authorization for prescription renewals was doubled to two years, and adaptations were broadened to include more medications. In 2024, pharmacists’ adaptation authority was expanded once again, to permit pharmacists to adapt prescriptions that have previously been adapted, and to include some adaptation authority for controlled substances to support harm reduction efforts.
As of October 2024, prescription renewals made up 88 per cent of all adaptations made by pharmacists, with nearly 84,000 prescriptions renewed in that month alone.
With the expansion of adaptation scope, the use of this service is expected to continue to grow, with the Ministry of Health providing $7.45 million in funding for the service in the most recent fiscal year, up 67 per cent from the year previous.
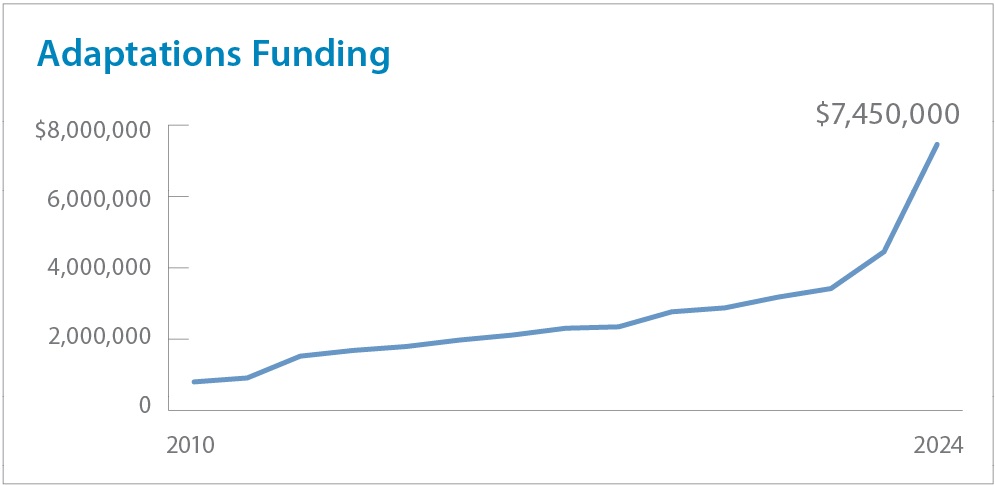
Funding data for pharmacy services is available through the Ministry of Health's PharmaCare Trends reports, available at: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-res…
Pharmacists’ involvement in treating Opioid Use Disorder
As early as 2004, pharmacists have been involved in the treatment of Opioid Use Disorder (OUD) through standards set by the College of Pharmacists of British Columbia. As dispensers of medications, pharmacists were initially involved in the daily witnessed ingestion of methadone, an opioid replacement. In 2016, physicians in British Columbia received authorization to prescribe Suboxone, a combination of buprenorphine and naloxone, and it was also around this time that Suboxone was covered as a regular benefit through PharmaCare, and Suboxone began being recommended as a first-line treatment for OUD as an alternative to methadone. A year later, Kadian, a slow-release oral morphine, was also covered by PharmaCare for the treatment of OUD.
In 2017, community pharmacies continued to become more involved in mitigating the opioid overdose crisis by participating in B.C.’s Take Home Naloxone program, where naloxone kits were distributed freely at pharmacies to people at risk of an overdose. Currently, nearly 900 community pharmacies distribute the kits.
In 2019, the BC Pharmacy Association, in partnership with the Ministry of Health, took on the role of creating and administering the training course, Opioid Agonist Treatment Compliance and Management Program (OAT-CAMPP) to raise the practice standard related to OAT-related services. OAT-CAMPP was the first course of its kind in Canada. Working together with the College, this training program was made mandatory. Additionally, with the onset of the COVID-19 pandemic, pharmacists were authorized to deliver OAT to patients directly, without having the patient come to the pharmacy, or authorize a regulated health professional to do the same. In 2023, OAT guidelines were updated to remove the ranking of OAT as first, second and third- line treatments, in favour of recommending collaborative decision-making based on clinical judgment, client goals and circumstances.
As of the end of 2024, more than 5,800 registrants had completed the Association’s OAT-CAMPP, which was also updated to meet the latest guidelines.
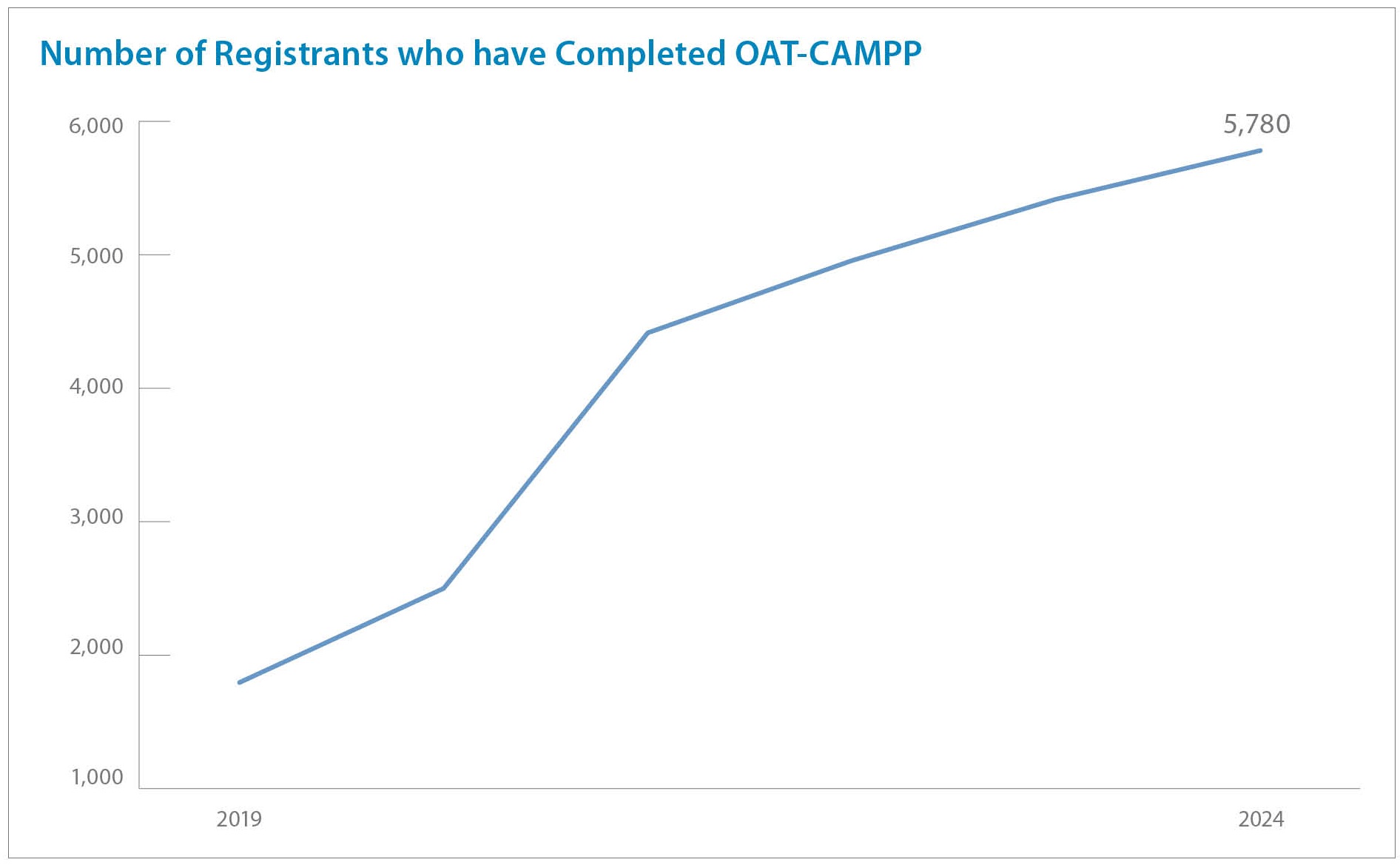
OAT-CAMPP, which is administered by the BC Pharmacy Association, was the first course of its kind in Canada.
Caring for seniors and those who take multiple medications
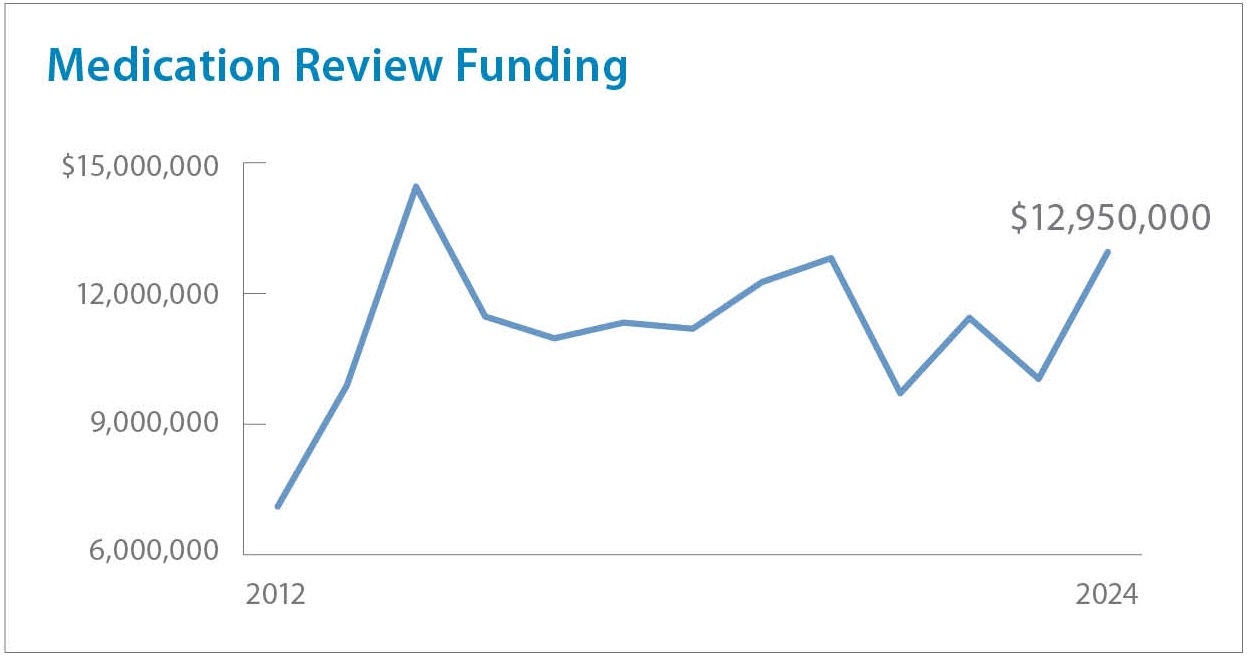
As medication experts with frequent contact with patient populations, pharmacists are uniquely positioned to assess whether patients are taking the best possible medication for their needs, or whether the mix of medications patients are taking may cause drug therapy problems. In 2011, British Columbia provided funding for pharmacists to conduct medication reviews with patients who have been dispensed at least five different medications in the prior six months. This service is available for a significant population of seniors, as it’s estimated that in Canada, 62 per cent of seniors are prescribed five or more medications, while 24 per cent of seniors are prescribed 10 or more medications, according to the Canadian Institute for Health Information’s 2021 data.
If a drug therapy problem is identified during a medication review, patients would take part in a discussion with the pharmacist to review the issue and have the pharmacist develop a plan to address it. Pharmacists will also follow up as necessary after the patient’s review. Since this program was launched in 2011, demand for medication reviews have remained relatively consistent, according to the Ministry’s funding levels for this service.
Prescribing authority for pharmacists arrives in British Columbia
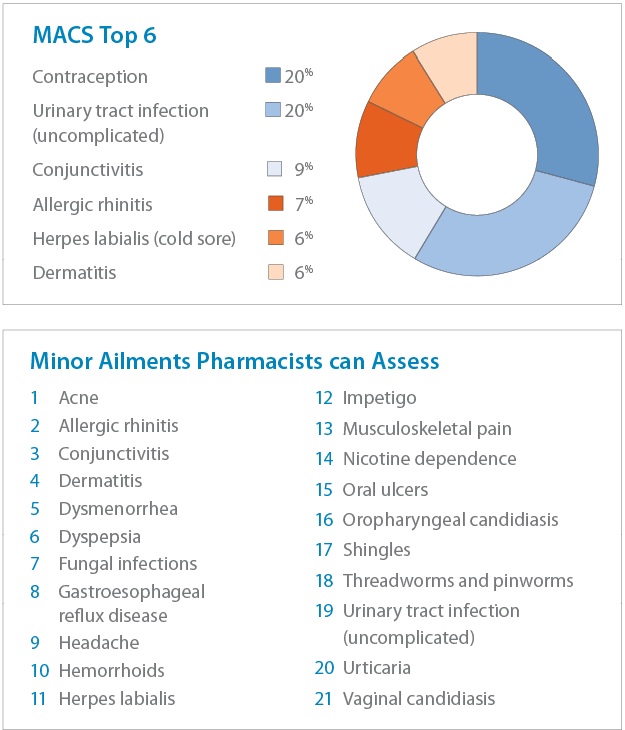
In June 2023, the pharmacist scope grew to include the authorization to assess and prescribe for 21 minor ailments, plus assess and prescribe for contraception. The selected list of ailments was intended to address conditions that can be readily diagnosed, and conditions that can reasonably be expected to be resolved with only short-term or episodic treatment. British Columbia also made headlines for being the first province in Canada to publicly fund contraception, and prescribing contraception is now the top prescribing service conducted in community pharmacies, making up about one-in-five visits.
Pharmacists graduating today have, for years, been taught how to assess and prescribe for minor ailments. Additionally, any pharmacist providing the service must complete a mandatory education module required by the College of Pharmacists of British Columbia. After the first year of the program’s launch, 92 per cent of the more than 1,400 pharmacies in British Columbia have provided minor ailments and contraception service (MACS) assessments, and 77 per cent of active pharmacists have provided at least one such service.
In the first year since pharmacists were authorized to prescribe, more than 312,000 patients visited a pharmacy for MACS, for a total of more than 431,000 assessments performed.
The latest MACS service numbers were published on July 31, 2025 and are available here: https://www2.gov.bc.ca/gov/content/health/practitioner-professional-res…
The profession is lean, but growing
As a profession, pharmacists have a demonstrated track record of increasing access to health care for British Columbians.
While community pharmacists have traditionally been the most accessible health professional — anyone can walk into a pharmacy, even on weekends, holidays or late at night — to seek advice or health needs, the profession is becoming ever more accessible. There are now more pharmacists, and more pharmacies, available as a proportion of the population than in the past 16 years.
Today, there is one community pharmacy for every 3,814 residents in British Columbia, compared to 4,336 in 2009, while there is one community pharmacist for every 1,341 people, compared to 1,571 in the past, using the same range of years.
As the province grows, community pharmacists will continue to be there for the public, as they have always been, while delivering excellent care and unparalleled value for the level of service they provide.
