By Michelle Gray, BSc(Pharm), RPh
Board Director, BCPhA

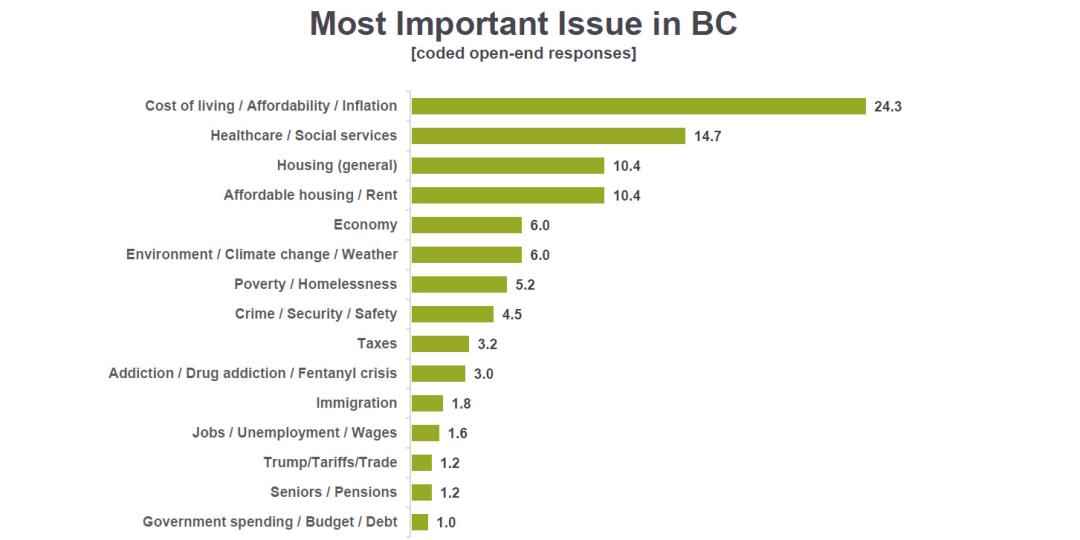
Recently, the BC Pharmacy Association commissioned a public poll to get the pulse of British Columbians, gauge their appetite to support the pharmacy profession, and to help inform the next steps of the Association’s advocacy plans. In the polling results, British Columbians identified health care as the second most important issue facing them today, just behind cost-of-living and affordability.
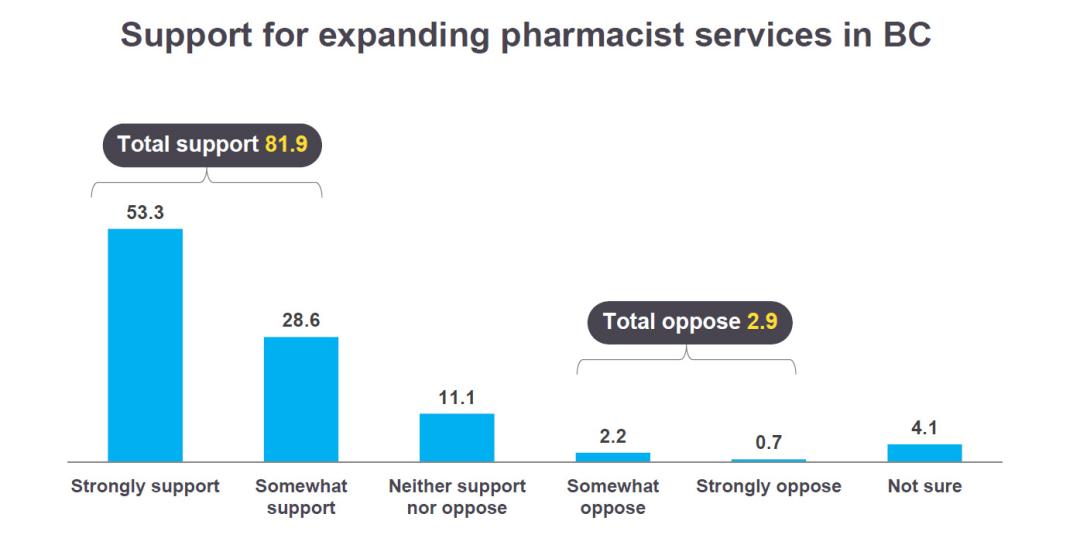
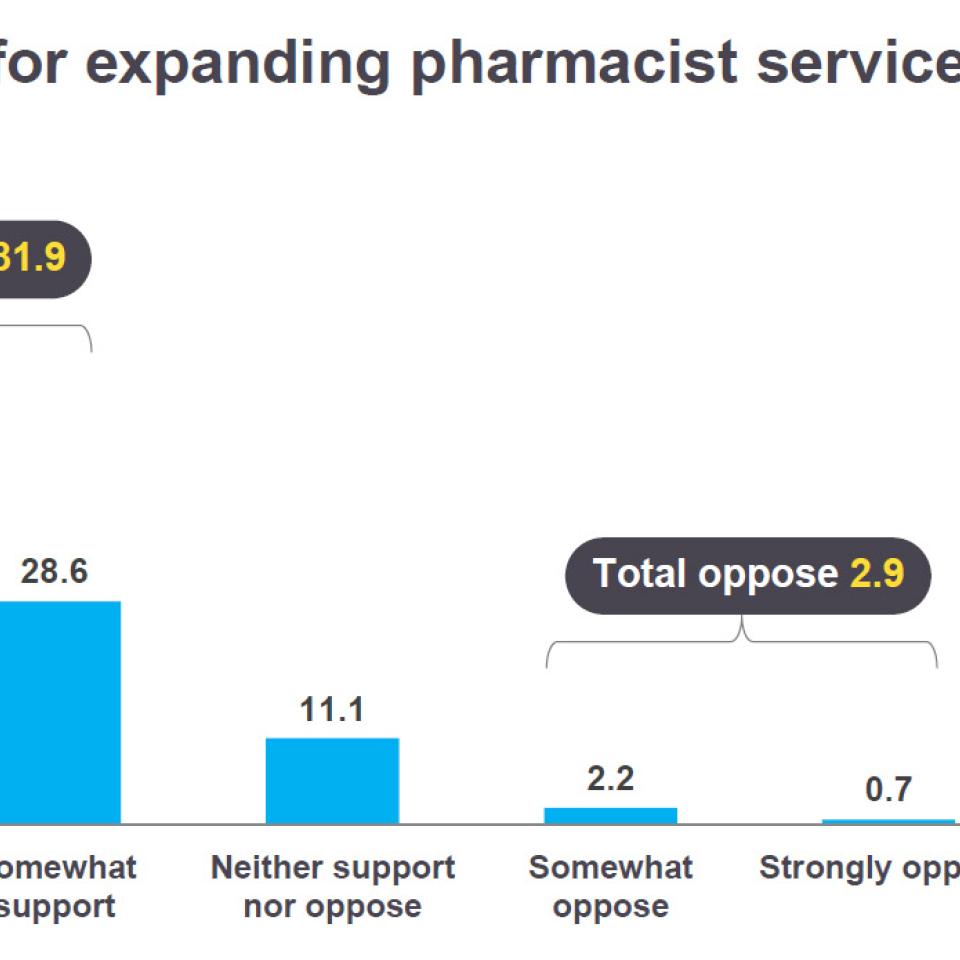
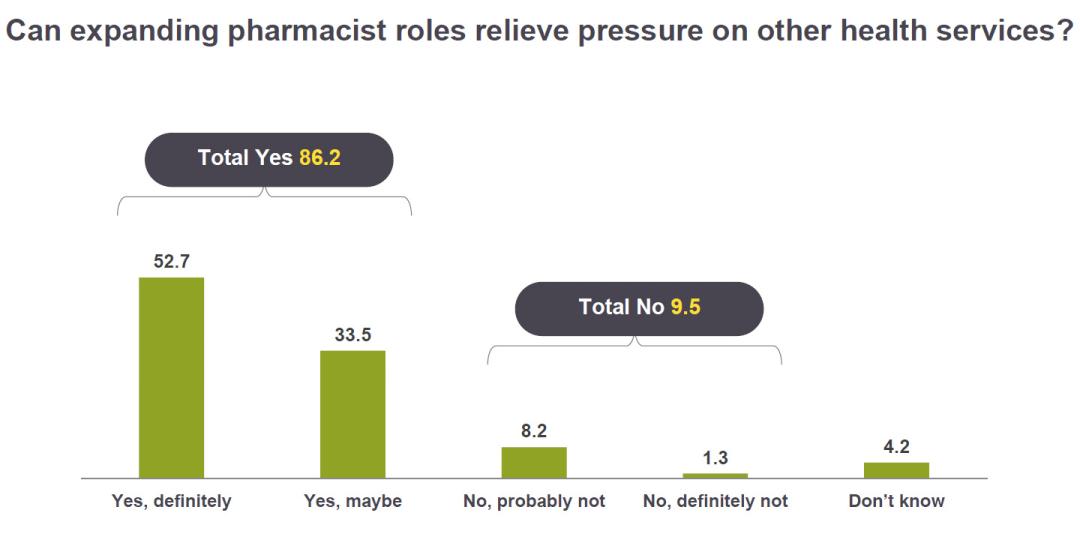
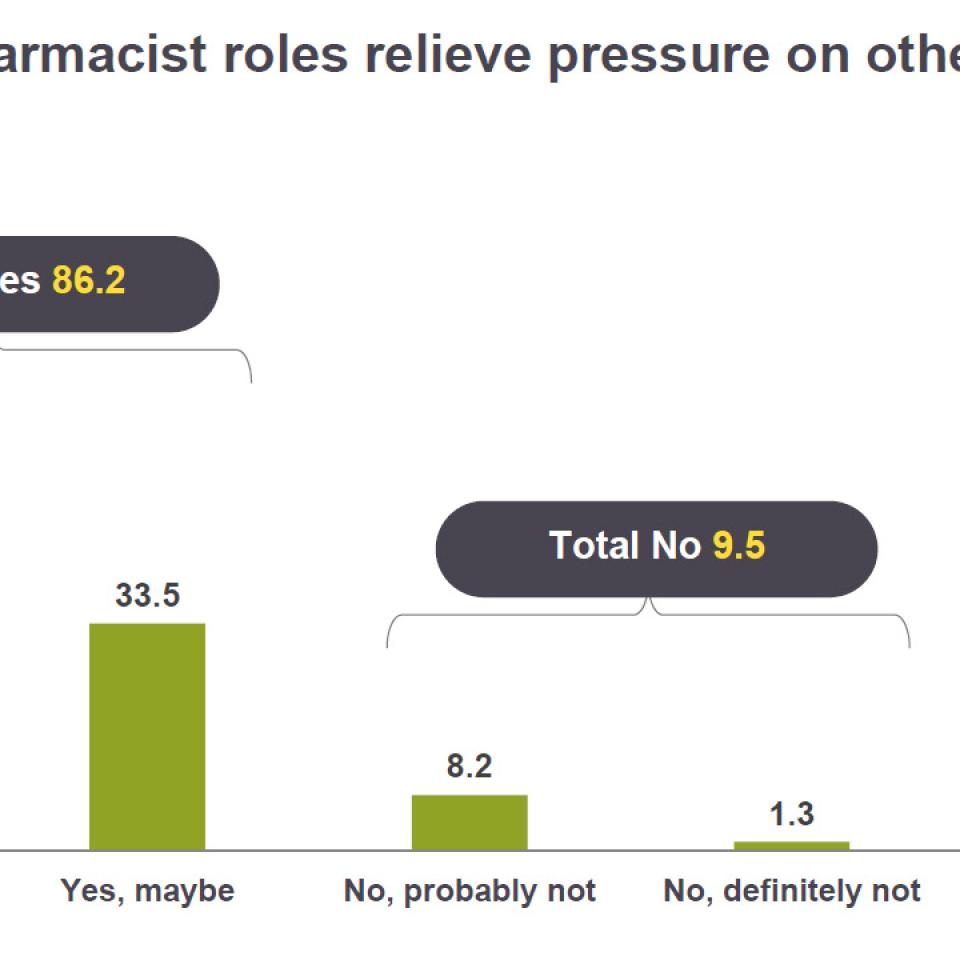
The results showed that the public sees the services provided by community pharmacists as crucial to maintaining access to health care in the province, and close to nine-in-10 members of the public would like to see an expansion in the types of services pharmacists offer.
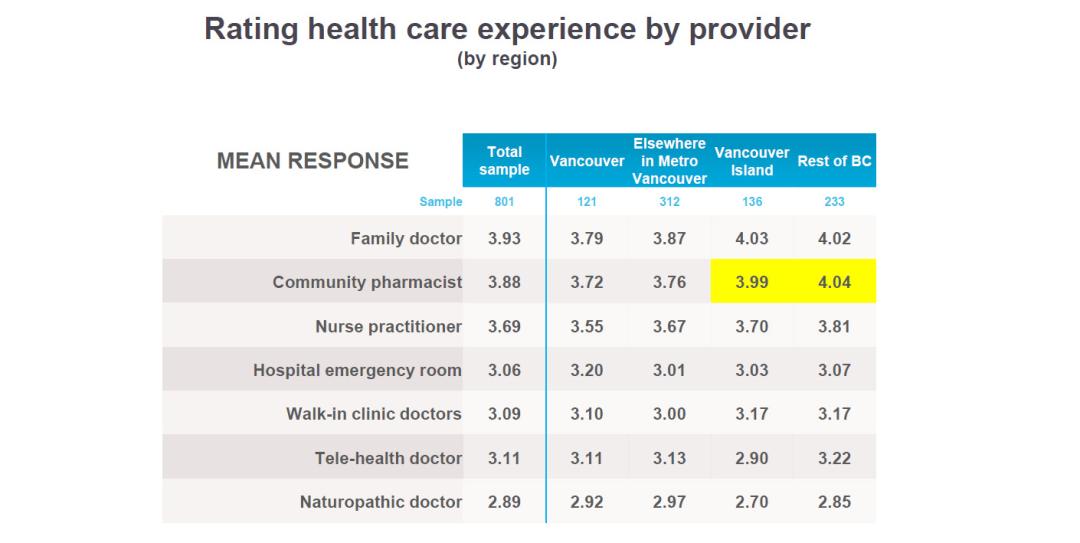
The data show that we are providing excellent care in the eyes of our patients. The poll asked patients to rate their experience on a scale of one to five by health-care provider, with five being the highest. Community pharmacists received an average score of 3.88 out of five, just behind family doctors who received an average of 3.93 out of five.
Pharmacists were ahead of nurse practitioners, hospital emergency rooms, walk-in clinic doctors, telehealth doctors and naturopathic doctors.
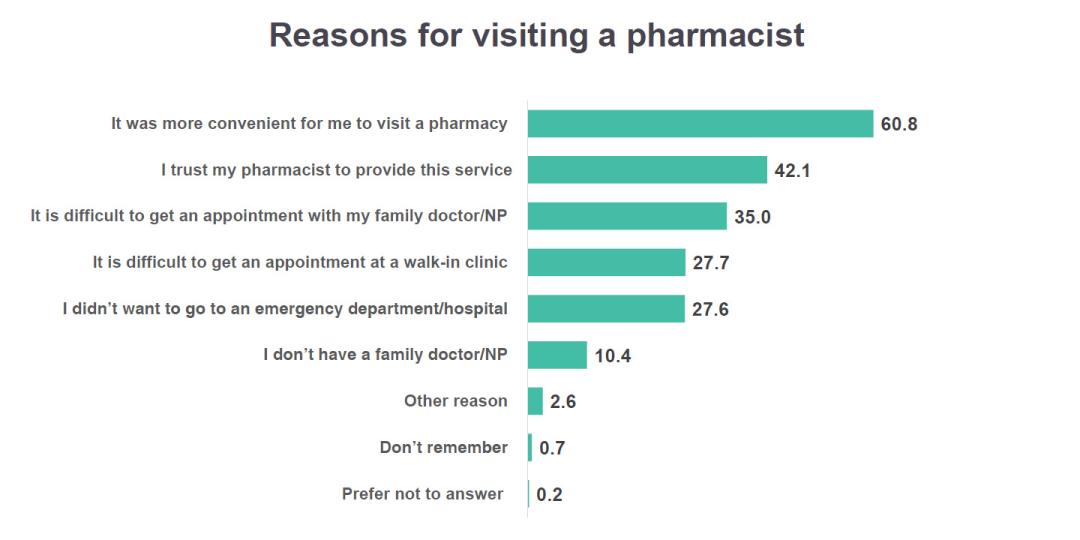
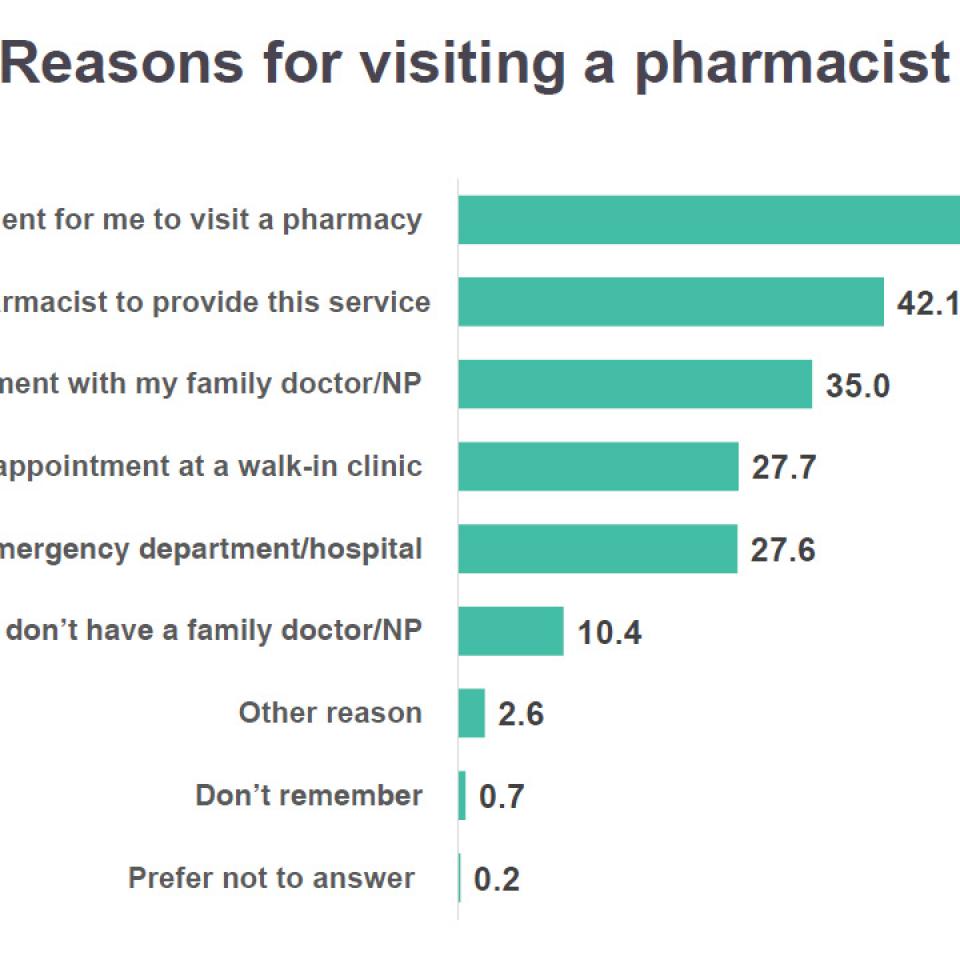
The data also show us that convenience is the primary driver for people visiting community pharmacies. Our pharmacies are in their communities; we’re always open; we are accessible without wait times; and we are offering an increasing number of services. Our accessibility and the convenience we offer is universally recognized. But we also know that patients see us because they trust us. Patients have always sought our advice to help navigate their health, and they know we are the providers who see them the most. We are able to see them quickly when patients need advice, even when other providers are not available right away.
The survey was conducted with 801 British Columbian adult residents from July 11 to July 18, 2025 by Stratcom.
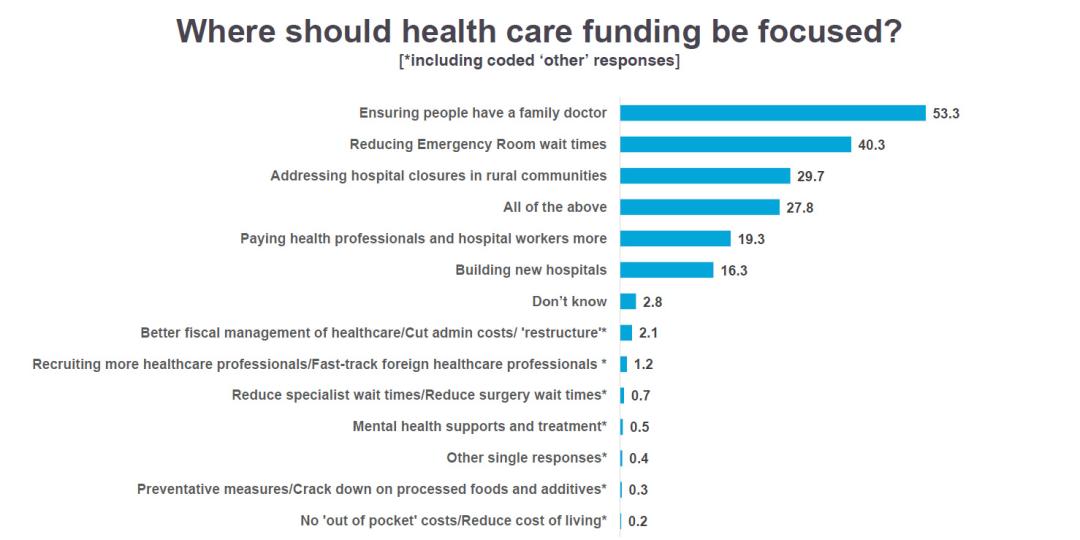
There is no doubt the public supports increased access to care. But where the challenge arises is their appetite for increasing funding for care. Affordability is their top concern by a significant margin, and when it comes to additional funding, the public overwhelmingly prefers that money go toward additional medical doctors, reducing emergency room wait times, and addressing hospital closures, and the data show few in the public are supportive of increasing financial compensation for any health profession — not just us. Just take a look at the ongoing negotiations and job action between public sector employees and layoffs at various levels of government that have been dominating the news lately.
So the question for us is, how do we get the needle to move for pharmacists?
Through our work at the Association, we continue to have conversations with the Ministry of Health and with provincial MLAs. It seems that there is an appetite to spend smarter, to invest in programs that would help reduce costs, while maintaining a proper level of service.
One example that governments have been looking at is the idea of funding pharmacy-led clinics. Additionally, there is opportunity for the government to look at expanding the list of minor ailments, opportunity in funding point-of-care tests that patients can have done at the pharmacy counter, and the opportunity to involve pharmacists in the interpretation of test results and health monitoring. By investing additional funds in community pharmacies, government could potentially realize savings and improve health outcomes for patients.
I know that increasing the core dispensing fee is something that is long needed for the profession. The dispensing fee has been a topic in almost all board meetings I have participated in over my four years of service on the Board of Directors at the Association. It is an important topic, and we are all in agreement that it needs to increase.
The last time the dispensing fee increased for B.C. pharmacists was in 2011, from $9.60 to $10 per dispense. That was the same year the minimum wage increased in B.C. to $8.75 from $8 per hour. The minimum wage today in B.C. is $17.85 per hour. Clearly, there is catching up to do.
While we have made a formal proposal to government to increase the dispensing fee, I also know that government works in cycles, and timing is key. What is also key is ensuring that we have a voice at the table in every cycle. Right now, the current cycle has the government facing substantial deficits while balancing cuts to the health-care system. We know that expecting the government to increase the dispensing fee in the face of a record-breaking projected deficit of $11.6 billion will likely be unsuccessful.
Despite these challenges, the pharmacy profession in British Columbia has been continually building stronger connections and relationships with key government officials, in no small part due to the Association’s efforts, to put us in a place where, when the cycle comes around once again, we are poised to make the case for financial support and new funding.
Any pharmacist knows that the cost of doing business has increased in the last 14 years. Even if the price of medications is unchanged, the costs of commercial property, of employing staff, of keeping the lights on and more, all that has increased significantly.
With that in mind, in September, the BCPhA Board voted to undertake an Activity Based Costing Study to assess the costs associated with dispensing a prescription in B.C. pharmacies. The aim of this study is to identify the current time and financial costs of services, and to identify any factors that might impact those costs, such as whether a pharmacy is in an urban or a rural area. With this information, it is hoped that our advocacy asks will be better guided by current data when we next meet with the provincial government.
What we know is that our collective efforts in embracing our expanded scope have made a difference in the lives of British Columbians. Consistently, our polling data show that utilization of pharmacy services and support for the profession is higher in areas outside of Metro Vancouver, areas which have been most impacted by lack of access to care and hospital closures.
As a pharmacist who practices in a rural area, I see this satisfaction daily in the patients who visit my pharmacy.
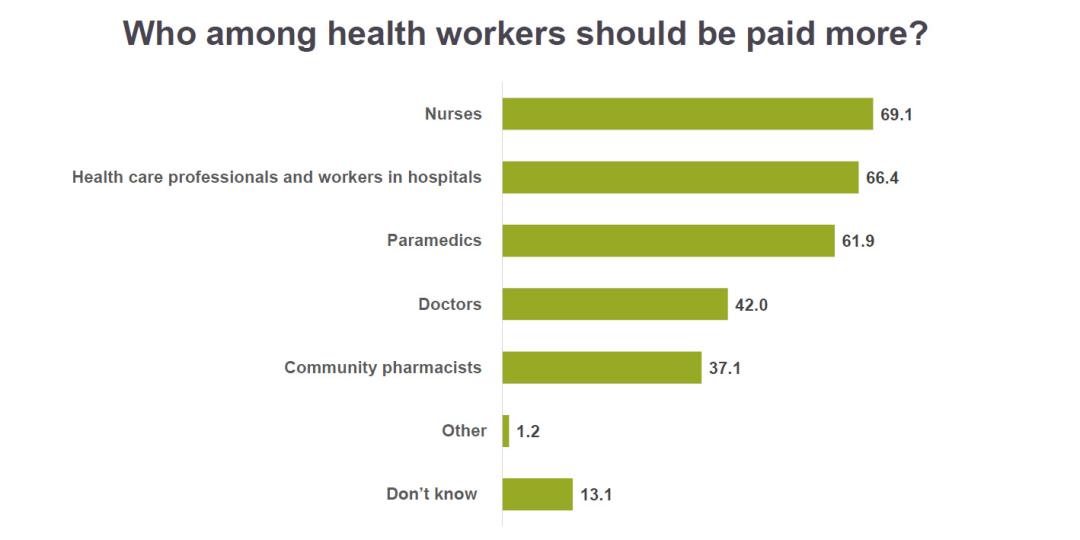
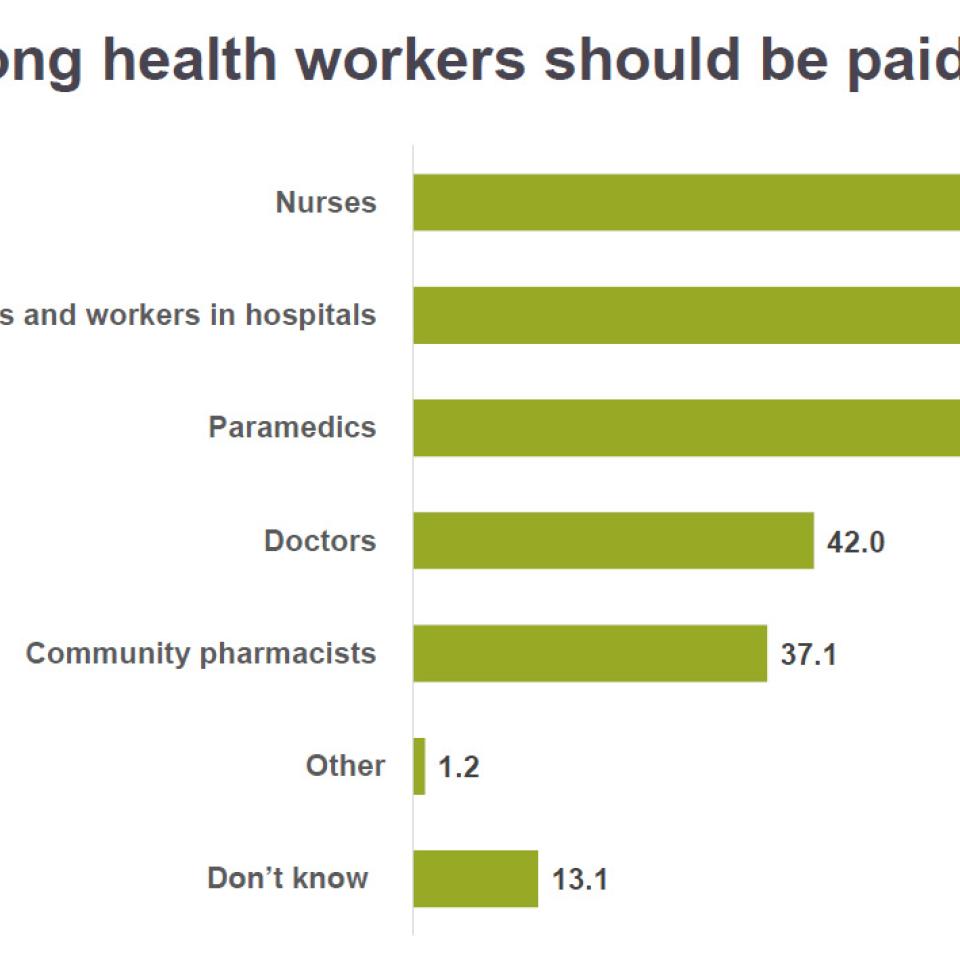
As health-care providers, we are an integral part of the health-care team, like nurses, doctors and other health professionals who all have important roles in caring for the health of our communities. But as community pharmacists, we often have more work to do when it comes to our public perception — the public by and large, at least according to our polling data, views us as private, commercial entities rather than as a part of the public health system. This means that even if the public were to support increasing wages for health professions, community pharmacists are not at the top of the list. Rather, the public believes it is nurses, hospital workers, paramedics and doctors who should be ahead in the line.
This means that we, as a profession, have more work to do when it comes to educating the public about community pharmacists’ role serving British Columbians. We do this at the counter with such actions as renewing a prescription when it’s appropriate and explaining the process rather than simply giving an emergency fill or explaining to patients that pharmacists have the ability to check records in CareConnect. If we simply view conversations as transactional, it’s unlikely to move the needle.
We operate under strict clinical and ethical standards, and our role is to service our patients and relieve pressure on the system. And it’s upon us to make sure our patients understand that we are a public health access point, and we deserve, and need, their support.