
For decades, medicinal cannabinoids have occupied an uncomfortable space in Canadian health care — widely used by patients, increasingly supported by evidence, yet structurally separated from the very professionals best trained to manage medications. The result has been a fragmented, confusing system that places unnecessary risk on patients and undermines the legitimacy of cannabinoid-based therapy as medicine.
If Canada is serious about patient safety, access, and accountability, it is time to ask a difficult but necessary question: Who should be responsible for the clinical oversight of medicinal cannabinoids? The answer, increasingly clear both domestically and internationally, is pharmacists.
From Stigma to Structure
Medicinal cannabinoids have long suffered from reputational baggage. As Manitoba’s Dr. Jennifer Anderson, MD (Physician, Keynote Speaker, Advocate, Expert and Educator in cannabinoid medicine and a mom to a Cannakid superhero), recently observed, many still picture the “authorizing physician” as a detached, transactional figure — someone disconnected from primary care, providing quick approvals without follow-up or accountability. While that perception is uncomfortable, it did not arise in a vacuum.
Across Canada, cannabinoid authorization has often occurred outside established circles of care, sometimes involving clinicians with no longitudinal relationship with the patient, no shared health record, and no ongoing monitoring. This model has reinforced the notion that medicinal cannabinoids exist outside “real medicine.”
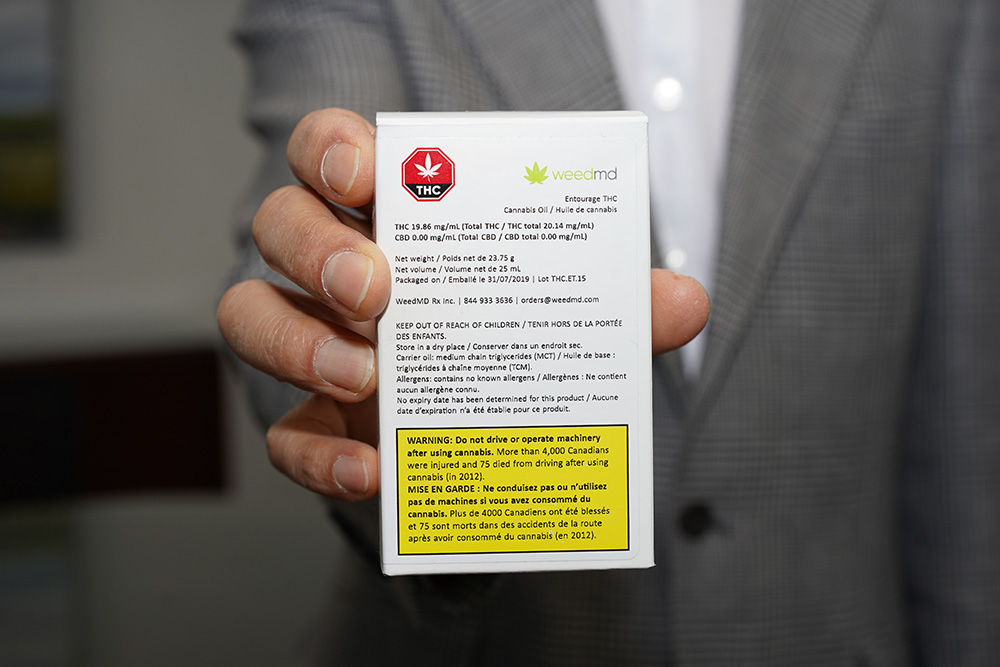
Yet cannabinoids are not fringe therapies. They are pharmacologically active compounds with known mechanisms, dose-response relationships, metabolic pathways, and clinically meaningful drug interactions. They should therefore be treated like other therapeutic agents: prescribed judiciously, monitored longitudinally, and integrated into comprehensive medication management. That is precisely where pharmacists excel.
Canada’s Convoluted Medical Cannabinoid Framework
Canada’s current medical cannabinoid program is, at best, confusing. Patients must navigate authorizations that feel disconnected from their regular care, while product distribution occurs almost entirely through mail order direct from licensed producers. Pharmacists — arguably the most accessible health-care professionals — are largely excluded from meaningful clinical involvement.
This has real consequences. Patients frequently self-titrate without guidance, misunderstand bioavailability differences between oral, inhaled, and topical formulations, or combine cannabinoids with central nervous system (CNS) depressants, anticoagulants, or psychotropic medications without adequate oversight. The system unintentionally promotes trial-and-error rather than evidence-informed care.
Ironically, this fragmentation persists despite long-standing recognition of the pharmacist’s role. The federal Health Canada Task Force on Cannabis explicitly recommended that cannabis be dispensed through pharmacies with pharmacist involvement. Yet more than half a decade later, policy has not caught up with practice.
Pharmacists: The Most Accessible Medication Experts
Pharmacists are uniquely positioned to manage medicinal cannabinoids because cannabinoids are, fundamentally, medications.
Pharmacists are trained in:
- Pharmacokinetics and pharmacodynamics
- Bioavailability by route of administration (oral, sublingual, inhaled, topical)
- Drug–drug and drug–disease interactions
- Dose titration, therapeutic monitoring, and adverse-effect management
- Patient counselling and longitudinal follow-up
These competencies are directly applicable to cannabinoid therapy. Whether managing THC-associated cognitive effects, CBD-mediated CYP450 interactions, or balancing efficacy with tolerability in chronic pain, pharmacists already perform analogous functions daily with other medications.
Just as importantly, pharmacists are the most accessible health-care professionals in Canada. Patients see them frequently, often without appointment, and across both urban and rural settings. This accessibility is critical for therapies that require careful titration, education, and follow-up.
Evidence-Informed Use, not a Magic Bullet
Medicinal cannabinoids are not a panacea. They are not appropriate for every patient or every condition. But dismissing them because they are imperfect ignores a growing body of evidence and real-world clinical experience. Medicinal cannabinoids have demonstrated benefit in:
- Chronic pain
- Chemotherapy-induced nausea and vomiting
- Appetite stimulation and cachexia
- Multiple sclerosis spasticity
- Rheumatoid arthritis and inflammatory conditions
- Parkinson’s disease symptom management
- Dementia-related agitation
- Menstrual pain and endometriosis
- Pediatric epilepsy, particularly refractory syndromes
Notably, repeated studies have shown that cannabinoid therapy can reduce opioid consumption, a finding with profound implications amid Canada’s ongoing opioid crisis. Estimates suggest that approximately 40 per cent of all cannabinoid use is health-related, spanning both formal medical authorization and wellness-driven therapeutic use.
Topical cannabinoid formulations are also increasingly prevalent, particularly for localized pain and inflammatory conditions — yet are often used without professional guidance despite their pharmacologic activity.

International Precedent: Pharmacists at the Centre
Canada is increasingly an outlier in excluding pharmacists from cannabinoid care. In countries such as Germany, the United Kingdom, Australia, and Switzerland, medicinal cannabinoids are managed within pharmacy-led or pharmacy-integrated systems. Pharmacists dispense, counsel, and monitor therapy as part of routine care.
The United States is also evolving. The reclassification of cannabis from Schedule I to Schedule III at the federal level is expected to move cannabinoid-based therapies further into mainstream medical and pharmacy management, aligning with controlled substance frameworks already familiar to pharmacists. International experience demonstrates that integrating cannabinoids into pharmacy practice increases accountability, normalizes their medical use, and improves patient outcomes.
Physicians, Pharmacists, and Shared Responsibility
This is not an argument against physicians. Nor is it a call to diminish their role. Physicians remain essential for diagnosis, overall care planning, and complex case management.
However, it is notable that in December 2024, the College of Physicians and Surgeons of Ontario withdrew its medical cannabis position statement. This withdrawal reflects ongoing uncertainty within the medical profession about ownership of this therapeutic area.
Rather than leaving a vacuum, Canada should embrace a collaborative model. Pharmacists already prescribe independently or adapt prescriptions for many conditions across several provinces. Extending this authority to medicinal cannabinoids — within defined parameters — is a logical progression.
A Pragmatic Path Forward: Prescribing Before Distribution
While many advocate for distributing cannabinoid products through pharmacies, doing so would require significant regulatory restructuring. Pragmatically, it may be faster and more achievable to first enable pharmacists to prescribe medicinal cannabinoids, even if distribution remains via direct-to-patient mail order in the short term.
This approach delivers immediate patient benefit:
- Clinical guidance at initiation
- Safer titration and monitoring
- Integrated medication reviews
- Improved documentation and follow-up
Patients become the primary beneficiaries, receiving professional clinical oversight without waiting years for wholesale system reform.
Start Small: A Pilot with Purpose
Change does not need to be sweeping to be meaningful. A limited pilot program allowing trained pharmacists to prescribe medicinal cannabinoids — under defined indications and monitoring requirements — could demonstrate value quickly.
Such a pilot could focus on:
- Chemotherapy-induced nausea and vomiting
- Chronic pain/arthritic pain
- Opioid-sparing strategies
- Neurologic conditions
- Palliative care
Outcomes could include patient satisfaction, safety metrics, opioid reduction, and healthcare utilization. Evidence generated from real-world practice would inform broader policy decisions.
Coverage, Cost, and Continuity
Medicinal cannabinoids are already recognized as legitimate therapy by some third-party payers, including private insurance plans, Workers’ Compensation Boards, and Veterans Affairs Canada. Yet the disconnect between coverage and clinical oversight remains striking.
Pharmacist involvement would improve continuity of care, documentation, and payer confidence — further reinforcing cannabinoids as medicine, not exception.
As Dr. Anderson rightly noted, medicinal cannabinoids do not need less medicine around them — they need better medicine around them. Legitimacy will not come from distancing cannabinoids from the healthcare system, nor from isolating their use in parallel structures. It will come from integration, accountability, and standards. Pharmacists are already embedded in Canada’s medication infrastructure. They are trusted, regulated, and trained for exactly this type of responsibility.
Conclusion: Time to Modernize
Medicinal cannabinoids are here to stay. Patients are using them. Evidence continues to evolve. International models are maturing. The only question is whether Canada will modernize its approach or continue to manage cannabinoids as an outlier therapy.
Allowing pharmacists to prescribe medicinal cannabinoids — within a collaborative, evidence-informed framework — is not radical. It is rational. For the sake of patients, safety, and the credibility of cannabinoid-based medicine, it is time to place medicinal cannabinoids where they belong: under the professional supervision of pharmacists.
About the Author:
John Tse is Vice President, Commercial Development at Light AI Inc., advancing smartphone-based diagnostic and wellness technologies, and Founder and CEO of 36Eight Technologies, a bioinformatics and pharmacological health company developing clinical decision-support systems for personalized medicinal cannabinoid care. Tse is a Director on the Board at the BC Pharmacy Association.
